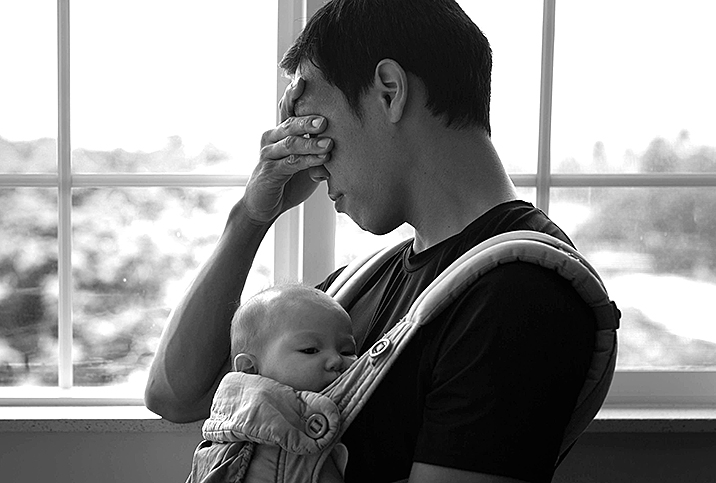
Men Get Postpartum Depression, Too
In 2019, Ryan Kuja's wife had triplets. A Michigan-based licensed therapist, coach and spiritual director, Kuja had struggled with depression for most of his adult life. Introducing his premature triplets into his life only intensified his depressive symptoms.
"There was a mix of anxiety associated with hyperarousal and depression, which is associated with another branch of the autonomic nervous system, the dorsal vagal complex," Kuja said. "For me, I'd be wound up in the chaos, experiencing excruciating symptoms of anxiety and stress, then I'd crash down into depression in a never-ending cycle. I knew the toxic amounts of stress was creating this cycle, but it seemed there was nothing I could do."
Many men don't know it's possible to have postpartum depression (PPD)—it's usually only talked about in the context of the parent who has given birth. However, the societal stigma surrounding it means many men suffer in silence, even when it's hurting both them and their families.
What's male postpartum depression?
PPD is an episode of major depressive disorder that happens after the birth of a child. It can cause symptoms such as irritability, restricted emotions and low mood.
While PPD can happen to any parent—and any dad—some people are at a higher risk than others. Parents with a personal or family history of depression and people living in poverty are more likely to get PPD. First-time dads are at a higher risk, too. Experts don't know exactly why this is, but according to the National Childbirth Trust (NCT) in the United Kingdom, the new responsibilities, changes in their relationship and money concerns can all play a role.
Male postpartum depression is not often the subject of media reports, but it's more common than you might think. A 2020 study published in Australasian Psychiatry indicated 12 percent of the dads they surveyed met the criteria for paternal PPD.
"If the mom has postpartum depression and [the father] isn't receiving his own help, his probability of developing depression is 24 to 50 percent," said Shoshana Bennett, Ph.D., a California-based psychologist and the author of "Postpartum Depression for Dummies."
Factors for men to develop PPD include sleep deprivation, worrying about losing the relationship with his wife or girlfriend, and financial concerns, she said.
What does it look like?
The symptoms of postpartum depression can be confusing and scary. While the condition affects many women, they tend to be more aware of the risk factors and often have a midwife or doctor checking them for potential warning signs of depression. But dads don't have these safety nets and can easily slip through the cracks.
"Postpartum depression in men often manifests as anger and/or withdrawal from family life," Bennett said. "For example, working longer hours or disappearing for long periods and playing video games are quite common."
Withdrawing from friends, being frustrated, feeling fearful, struggling to sleep, and using drugs and alcohol can be other commons symptoms.
Who is at risk?
According to the NCT, first-time dads and those ages 25 and younger may be more likely to develop PPD. Other risk factors include having a history of anxiety and/or depression, experiencing financial pressures, and not being in a relationship with the baby's mother.
It's not entirely clear what causes postpartum depression, but experts think hormones play a major role.
Self-imposed stigma can play a role in PPD, according to Chicago-based psychologist Steve Cisneros, Ph.D.
"I've worked with men who have had the thought, 'I went from being a lawyer or an accountant, a trainer, a mechanic, etcetera, to this?' which doubts their ability, reinforcing the depression cycle," he said.
After a person gives birth, their body goes through huge hormonal changes. But many people don't know parents who don't give birth experience hormonal changes, too. They might have raised levels of cortisol, the stress hormone, and vasopressin, which regulates sleep. While all these changes can help a new parent bond with their baby, they can also increase their chance of developing PPD. Basically, anything that adds extra stress to your life can increase your chances of PPD, which may explain why it's somewhat common.
Being sleep-deprived and waking up for late-night feedings is part of having a new baby, and it's something nearly every parent experiences.
A 2018 study published in Sleep Medicine Clinics found a link between sleep deprivation, disrupted sleep and postpartum depression. This isn't surprising—and it's also not useful. Being sleep-deprived and waking up for late-night feedings is part of having a new baby, and it's something nearly every parent experiences. In particular, PPD can significantly impact people without robust support systems, time off work and affordable childcare options.
But while some of these risk factors can make you more likely to get PPD, none of them guarantee it. Likewise, you can get PPD even if you don't have the risk factors.
According to another 2018 study, research shows conflicting results on which factors increase a person's risk and which ones don't. This is important to note, and it shows postpartum depression is a result of a complex combination of factors, individual characteristics and more. It's not easy to predict and it's also not your fault for getting it.
Getting help
If you're a father who is feeling the symptoms of postpartum depression, it's important to seek help.
"Children need both parents to be emotionally healthy," Bennett said. "The focus is now shifting from only maternal mental health to parental mental health. Reaching out to a therapist who specializes in dad depression can be a wonderful first step."
Cisneros recommended that people do their best to convey their feelings to health professionals and loved ones.
"Dads can get help by talking with trusted friends, their spouse or by reaching out to their primary care provider," he said. "Most PCPs have seen this before and can refer them to a specialist or give appropriate medication."
Unfortunately, PPD in men is understudied, so there isn't a lot of research on what treatment methods are best. Usually, the treatment protocol is similar to that for PPD in women and involves a combination of medication and therapy.
"Traditionally and culturally, men are supposed to simply handle their emotions and remain solid rocks and, therefore, rarely acknowledge depression of any kind," Bennett explained. "Plus, since they don't birth babies and their hormones are not involved as they are in the moms, it was assumed that they could not be affected by depression. For these reasons, until quite recently, new-father depression had not been taken seriously."
Being a parent is hard work, and sometimes, dads can feel forgotten. Kuja's recovery is ongoing.
"My little ones are 2½ years old, and the toddler stage is also grueling," he said. "I have gotten better at self-care and practices to regulate my nervous system, as well as taking time away regularly for retreat, rest and relaxation, where I can be away from the children for a few days. That has been hugely beneficial."


















