How to Manage Vulvar Dysplasia

Too few of us understand or know the correct terminology for the vulva, meaning conditions that affect it are rarely discussed, let alone accurately.
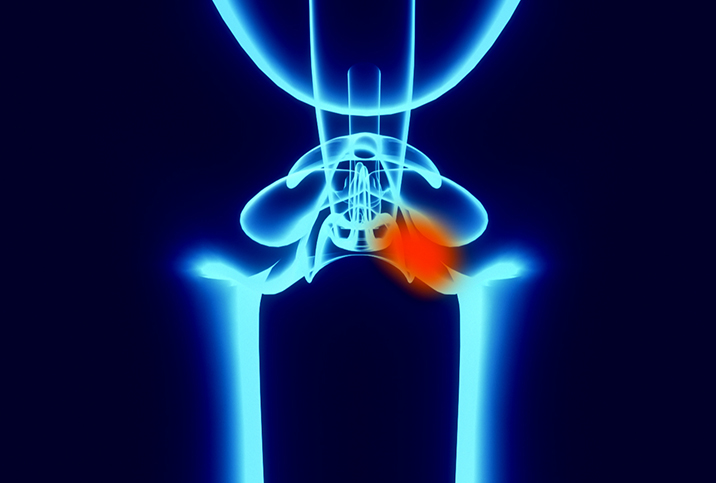
Vulvar dysplasia, or vulvar intraepithelial neoplasia (VIN), is one of them. This little-known nuisance is usually seen in women in their 40s.
"Vulvar dysplasia, or vulvar intraepithelial neoplasia, is a growth of precancerous cells on vulvar skin," said Rugilė Kančaitė, M.D., an obstetrics and gynecology resident based in Lithuania, and a medical advisor for Flo Health, an app to track periods and ovulation. "The presence of these cells is not cancer, but it deserves medical follow-ups and attention, as in some cases—not always—it can evolve into one."
Vulvar cancer is rare, occurring in 2.6 per 100,000 women in 2019, as reported by the Centers for Disease Control and Prevention (CDC). However, VIN is now four times more common than it was in the 1970s, according to the U.S. Surveillance, Epidemiology and End Results program. It is unclear if the change is connected to higher diagnostic rates or an overall increase in cases.
How does vulvar dysplasia present?
Vulvar dysplasia describes the appearance of abnormal cells on the vulvar layer's surface tissue. If a case is more serious, it's called VIN, which is divided into two subsections: low-grade and high-grade. High-grade cases are associated with a higher risk of progressing to cancer.
Typically, VIN can be cured with treatment, but if left untreated, it can progress to vulvar cancer. Even though this is usually a gradual process that takes well over 10 years to develop, consulting a physician about skin changes as soon as possible is necessary.
Itching, burning sensations and changes in vulvar skin texture or color all may be symptoms of vulvar dysplasia, Kančaitė said.
"Vulvar dysplasia is not cancer yet, but it has to be followed up carefully with a doctor to minimize the chance of developing into cancer or spotting it early," she said. "Keeping an eye on these lesions can help spot an early stage of cancer and begin treatment as soon as possible."
Triggers and treatment
"Most people probably know that human papillomavirus infection can lead to cervical cancer, but this little sneaky virus can cause vulvar dysplasia, too," Kančaitė said. "However, not all types of HPV can cause cervical and vulvar cancer, just a few. Cigarette smoking is another factor strongly associated with vulvar dysplasia. Vulvar dysplasia is more often found in people with lower immunity, such as people with autoimmune diseases or infected with HIV."
Vulvar cancer typically occurs in people with vaginas who are older than 70 and is generally more common in those older than 50.
Managing vulvar dysplasia depends on the type and whether it does develop into a type of cancer. Treatment plans vary depending on the case's severity and the patient's choices.
"Dysplasia, or vulvar intraepithelial neoplasia, in some cases, can be treated by laser and surgical therapy or by applying a special cream to the skin," Kančaitė explained. "Vulvar cancer treatment varies depending on overall health status and how advanced the illness is. Options may include chemotherapy, biologic therapy, radiation therapy and surgery."
Side effects, such as vaginal dryness, are managed by using external lubricants made explicitly for the vulva. In select cases, physicians may consider prescribing estrogen therapy to alleviate symptoms.
Look after your vulva
There are no specific guidelines on how often you should conduct a vulva check, but a semi-regular check should be a part of everyone's routine.
"I would say after every period it is always good to check things," said Susanna Unsworth, M.A., M.B., a gynecologist based in Cambridge, England, and a women's health expert for Intimina. "Get into the habit of regular checks of the breasts and vulva. Use a mirror and have a good look to see what is normal for you."
Alongside self-checks, regular OB-GYN appointments are important, even when you do not have any complaints. Taking care of your vulva should be fairly low maintenance. It does need any scented products or a daily in-depth physical exam.
"Scented feminine products can irritate the delicate skin and mucosa of the vulva and trigger thrush, bacterial vaginosis and vaginal dryness, which is also triggered by menopause, breastfeeding, and certain medications and contact dermatitis," Kančaitė said. "The vulva should be washed with warm water and patted dry."
Since VIN and vulvar dysplasia can be caused by HPV, vaccination decreases the risk of developing either condition.
"Ideally, girls aged 11 to 12 should be vaccinated, but it's not too late to catch up through age 26, even if they already had their sexual debut," Kančaitė advised. "Smoking is also a risk factor for vulvar dysplasia, so it's best to quit. Risk of HPV infection, trichomoniasis, genital herpes can be decreased by condom use."
Communication about the vulva is not vulgar
Any vulvar issue is undoubtedly impacted by the associated stigma, so learning to advocate for yourself is the most important step to protecting vulva health.
"Women should not feel ashamed of their bodies and should be able to speak freely if there is a problem," Unsworth said. "Most conditions can be effectively treated if caught early. Fear or shame should not be a reason for someone to not access help and risk more serious consequences."
If you have a health concern but are wary of reporting it, do not be afraid to ask for accommodations. Physicians are there to help, at your pace.
"Consider writing it down beforehand if you are struggling to speak [or] use words to describe," Unsworth said. "Access help in stages; [it] might be just talking about it is the first step. Then return another time for an examination so you are prepared for what will happen. Ask for it to be explained beforehand."
Vulvar dysplasia, or VIN, may be a rare condition but that should not negate the needs of its patients. It's time to let the stigma die and make vulvar health a priority for women and doctors alike.