Kick-Starting Your Sex Life After Vulvar Cancer

Medical recovery is nearly always a long, frustrating process, and oftentimes, reengaging with sex is a low priority.
This tendency to deprioritize sexuality after intense medical interventions increases when reckoning with the fallout of a condition that affects the genitals.
Vulvar cancer accounts for nearly 6 percent of cancers of the female reproductive organs and 0.7 percent of all cancers in women, according to the American Cancer Society (ACS).
Unfortunately, due to its location in one of our most intimate areas—and, perhaps, its rarity—few people openly discuss vulvar cancer's impact on a person's well-being and sexual function.
But it's important to understand the disease's impact on someone's sex life and, maybe even more so, how to help restore that sexuality.
What is vulvar cancer?
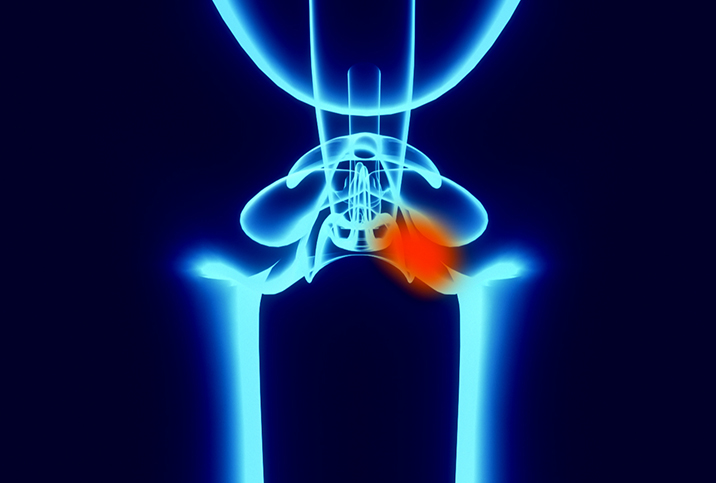
"The vulva contains the external structures of the female reproductive system," explained Clare Bertucio, M.D., a radiation oncologist and the founding chief medical officer of Medicine Mama's Apothecary in Laguna Beach, California. "It acts as a gateway and functions to help protect both the urinary and the reproductive system entrances."
Not only made up of the labia majora and minora—the folds of the skin that cover and protect the rest of the vulva—it encompasses several other parts. The vulva includes the mons pubis, which is the top of the pubic bone and is covered with a layer of hair; the vestibule, containing the openings to the urethra and vagina; and the clitoris.
The vulva also includes two types of glands, the Bartholin's glands, located on either side of the vagina's opening, and the Skene's glands, which are on each side of the urethra and help lubricate the vagina.
Cancer of the vulvar occurs on the outer surface of the genitalia. It occurs only in people assigned female at birth.
According to the ACS, an estimated 6,470 cases of vulvar cancer will be diagnosed in 2023, and about 1,670 women will die from the disease.
In instances where the cancer has not spread beyond the vulva, the disease has a five-year relative survival rate of 86 percent. For cancer that has spread to nearby lymph nodes or tissues but not distant organs, the survival rate drops to 53 percent, according to research gathered by the ACS. The survival rate is 19 percent if the cancer has spread to distant parts of the body.
"The average age at diagnosis is 65 years of age," Bertucio said. "Smoking, HPV infection, certain immune-compromised conditions, history of precancerous lesions of the vulva and certain skin conditions, [such as] lichen sclerosus, can increase a woman's risk of vulvar cancer."
Symptoms, treatment and prevention
"Warning signs of vulvar cancer may include persistent itching, pain, bleeding which is not associated with a normal period, lumps, open sores, unusual discharge, discolored skin patches, new growth of some sort, pain with urination, swelling in the vulvar area, any persistent new change, pain with intercourse or ulceration," Bertucio explained. "If you note any of the above, please see your healthcare provider immediately."
The diagnostic process for vulvar cancer involves a thorough physical exam followed by a colposcopy, which is a procedure for closely examining the vagina and vulva for signs of disease. Doctors then take a biopsy of anything that looks unusual.
This process determines the scope of treatment required, as Bertucio described.
"In very early-stage disease, local surgery may be enough, but in later-stage disease, more extensive surgical procedures may be necessary," she said. "Sometimes it is appropriate to sample a draining lymph node to make sure that disease has not spread to these tissues. Again, depending on the stage and extent of the disease, radiation and chemotherapy may play a role in treatment."
As with all cancers, the earlier vulvar cancer is identified, diagnosed and treated, the greater the chances of less invasive treatment and long-term survival.
Getting up close and intimate with your vulva on a regular basis is a crucial part of prevention, Bertucio said.
"If you do not touch and view this beautiful and sensitive part of your anatomy, you may miss an early warning sign of cancer," she advised. "Vulvar cancer screening is just one of the many reasons every woman should have a yearly exam with her healthcare provider.
"Part of loving yourself is being in touch—literally and figuratively—with your whole self," Bertucio added.
How does vulvar cancer impact sexual function?
"Depending on the extent of treatment needed, therapy for vulvar cancer may have a large impact on sexual function," Bertucio said. "Extensive surgery can result in loss of part or all of the vulva and/or surrounding tissue. This may not only result in a physical change in sexual function, but have a significant psychological effect on intimacy as well."
Vulvar cancer inflicts a toll on a person's overall well-being, and retaining a strong support network can be vital. Do not be afraid to reach out for help. Your treatment center can signpost resources to manage the impact.
"Radiation can also change the texture of vulvar and vaginal tissues, often creating severe dryness and potential narrowing and stiffness to the vagina," Bertucio added. "This can not only lead to significant discomfort and pain with intercourse but create very challenging emotional barriers."
Reentering the world of sex after vulvar cancer
The first step toward reengaging with sex after or during treatment for vulvar cancer is to determine if you are physically and emotionally ready.
A medical team is there to help you, so speak up and ask if they are ready to sign off on you physically. Your emotional readiness is up to you. Take some time to reflect on your mental state and assess if it is the right time to restart your sex life. Do not allow pressure to satisfy a partner's needs rush you into it.
"For women who have been treated for vulvar cancer and are experiencing side effects related to sexual function, we do try to offer as full an array of help as we can," Bertucio said. "Most cancer centers have sexual function workshops and groups that can be very supportive in this situation."
These centers can offer various interventions, including external and internal lubricant, pelvic floor therapy, vaginal dilators and counseling. The process is different for each patient.
"For each woman, an individualized program is designed to help return her and her partner, if relevant, to a new 'normal' level of sexual function and intimacy," Bertucio added. "Sometimes it is helpful to bring experts into the conversation to help explain and facilitate a potentially difficult discussion if either partner does not feel fully able to openly engage in this dialogue."
Communication
Engaging professionals to act as communication conduits can help couples rebuild their sex life safely, especially as open discussions around sex are already difficult for most people.
Before physically reengaging with a partner, explore yourself. Rediscover your body on your own terms first. Parts of your anatomy may have changed, and it's important to refamiliarize yourself before sharing.
"I would encourage counseling with a specialist in this area and participation in a support group," Bertucio said. "This is a very real and devastating consequence of some vulvar cancer therapy. Support, compassion and guidance are very important in navigating this often overwhelming and life-changing side effect of therapy."
Above all, be ready to share openly and honestly with partners about how vulvar cancer has changed your body, and keep an open line of communication while rebuilding.
There is no magic recipe for reigniting your sex life after vulvar cancer. The journey is far from linear. It's important to be patient and trust the process.