Though Rare, Vulvar Cancer Is a Disease Women Should Know

Many people have a general idea of what ovarian cancer and cervical cancer are, or have at least heard of them. However, vulvar cancer is a lesser-known disease that can affect women.
American Cancer Society statistics suggest that women in the United States have a 1 in 333 chance of developing vulvar cancer in their lifetime. This disease is expected to kill an estimated 1,670 American women in 2023, according to the ACS. The five-year relative survival rate is 86 percent when vulvar cancer is detected in the localized stage. But the rate falls off drastically when cancer has spread regionally (53 percent) and distantly (19 percent).
Learning more about its symptoms, diagnosis and treatment is vital to recognizing and preventing vulvar cancer.
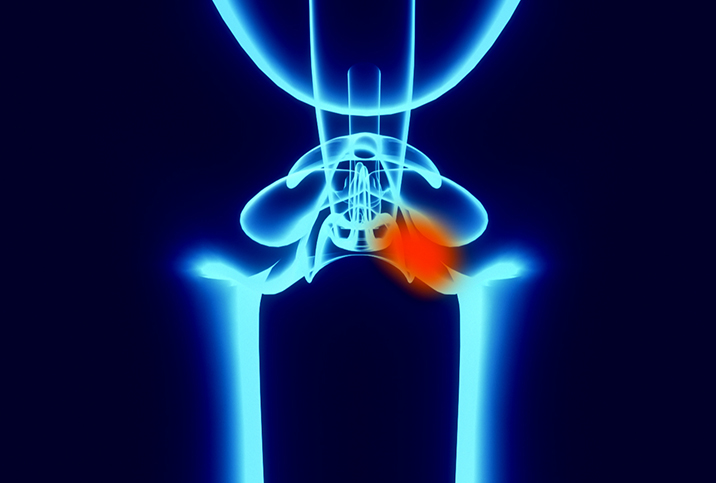
What is a vulva?
Before discussing vulvar cancer, it is important to understand the basics of a vulva. The vulva is the outside of the female genitals, including the labia majora, labia minora and clitoris. It is not the vagina.
"The vulva, or what some women refer to as their 'bottom,' is the area on the outside, around the opening to the vagina. It extends upwards to the clitoral area and the mons and towards the rectum in the posterior area," explained Mary Jane Minkin, M.D., a gynecologist and clinical professor of obstetrics, gynecology and reproductive sciences at the Yale School of Medicine in New Haven, Connecticut.
Symptoms of vulvar cancer
Vulvar cancer can manifest in a variety of ways.
"Vulvar cancer often presents with itching, skin that appears lighter or darker than usual, a bump or lump, pain or burning, bleeding or discharge, and/or an ulcer or sore that does not heal," said John P. Diaz, M.D., the chief of gynecologic oncology at the Miami Cancer Institute.
It can be easy to downplay these symptoms and assume they may go away with time. However, they could be a warning sign that you should be examined by a medical professional.
"The symptoms that most folks overlook is itching—they just think it's a bad yeast infection," Minkin said. "But if you are repeatedly treating yourself for a yeast infection and it just doesn't get better, do go to see your GYN provider."
Some patients may overlook a bump or open sores as well, according to Diaz.
People shouldn't assume they know how they developed vulvar cancer. The disease doesn't always come from the human papillomavirus (HPV) infection, according to Allison K. Rodgers, M.D., a gynecologist and reproductive endocrinologist and the director of education at Fertility Centers of Illinois.
"This is not true, as other skin cancers, like melanoma, can occur in the vulva," Rodgers explained.
Diaz noted that many women who have undergone a hysterectomy often think it's less important for them to see their gynecologists regularly and take preventive measures, which is a false assumption.
Diagnosis and testing
"While you cannot self-diagnose, it is important to know your vulva," Diaz said. "It is better for you to be able to demonstrate the changes to your vulva rather than simply relying on your gynecologist to notice any subtle changes to your vulva."
It is important to know your own body.
"A diagnosis may be given after a patient undergoes a biopsy, which is usually conducted in an office with a small amount of novocaine applied to the area," Minkin explained.
Further tests could be necessary to check the spread of the cancer. They might include:
- Colposcopy. Checks for abnormal cells in the vagina.
- CT or MRI scan. Checks for cancer in other body organs.
- Cystoscopy. Examines the bladder.
- Lymph node biopsy. Checks if cancer has spread to your lymphatic system.
- Pelvic examination under general anesthetic. Thoroughly looks at the internal reproductive organs.
- Proctoscopy. Looks at the inside of the rectum.
- X-ray. Checks if cancer has spread to your lungs.
Treatment and life after diagnosis
Treatment and recovery are not a one-size-fits-all or linear experience for everyone.
"The treatment for vulvar cancer varies, from surgery to radiation, chemotherapy or a combination of these treatments," Diaz said. "Depending on which therapy is required, this will determine what, if any, impact vulvar cancer may have on a patient's daily life.
"Side effects from surgery may include difficulty with wound healing, lower extremity swelling, difficulty with urination, decreased sensation, dryness and other side effects that may be related to chemotherapy," Diaz added. "Most of the time, these side effects are temporary and depend greatly on which treatment the patient undergoes."
Preventing vulvar cancer
Although engaging—or not engaging—in certain activities may not entirely prevent you from developing vulvar cancer, you can do certain things to help protect yourself and minimize your chances.
"There are two fabulous ways to protect against vulvar cancer," Minkin explained. "Never have unprotected sex with a new partner who has not been tested for HPV. HPV transmission is the most common way to develop vulvar cancer. And the other is stop smoking. Smokers have a much higher incidence."
"There is growing evidence that there may be a familial trait where women cannot clear high-risk HPV infections," Diaz added. "Those women who are unable to clear the infection are at increased risk of developing HPV-related cancers like vulvar cancer."
Getting vaccinated against HPV and routinely visiting a gynecologist are also critical steps. However, Diaz recommended seeing a doctor—even between scheduled visits—if you notice any of the symptoms discussed above.
Although vulvar cancer isn't as widely discussed among the general population as other cancers, it is still a disease that affects almost 6,500 people a year in the U.S., according to the ACS.
Taking the necessary measures to learn about your vulva, the symptoms of vulvar cancer and how to prevent the disease is critical.