Electronic Devices Could Help You Manage Your Period Pain
While some menstruating people do just fine with a heating pad and rest, others experience more extreme PMS symptoms. For those who experience high levels of pain and discomfort, and have tried all the tricks and remedies under the sun, electronic devices might be an option.
Sophia Yen, M.D., M.P.H., who is board-certified in adolescent medicine and is co-founder of Pandia Health, suggested traditional period pain management is a good place to start, with the option to move on to other methods if these tried-and-true ones don't work.
"If your period pain is causing you to miss school or work, please talk to a doctor," Yen advised. "We can start with ibuprofen 600 mg (with food)...up to three times a day for up to five days in a row (assuming you don't have kidney problems or other contraindications). If that doesn't work, then you can consider using the hormonal IUD, birth control implant, shot, ring, patch or pill to help lessen your period pain or stop your period entirely."
Kecia Gaither, M.D., MPH, FACOG, a double board-certified OB-GYN, echoed Yen's assessment, adding most treatments for period pain, or dysmenorrhea, involve the use of aspirin, or NSAIDS. These meds can have side effects or may not be recommended for certain patients, and as such, electronic devices can be utilized as a noninvasive and drug-free option.
What are electronic devices for period pain?
"TENS, or transcutaneous electrical nerve stimulation, is a methodology utilized to assist in alleviating pain, but the success of such is variable among individuals," Gaither explained. "The treatment is considered a form of alternative medicine.
"It involves placing small electrodes, which conduct electricity, with adhesives on the affected area," Gaither continued. "The electrodes are attached to a machine that releases electricity, sending impulses to the affected area."
It is said the electrical stimulation increases the levels of endorphins—the feel-good hormones—which serve as the body's own natural painkillers.
It's believed TENS works because the electrical impulses interrupt the messages pain receptors are sending to the brain. Additionally, it is said the electrical stimulation increases the levels of endorphins—the feel-good hormones—which serve as the body's own natural painkillers.
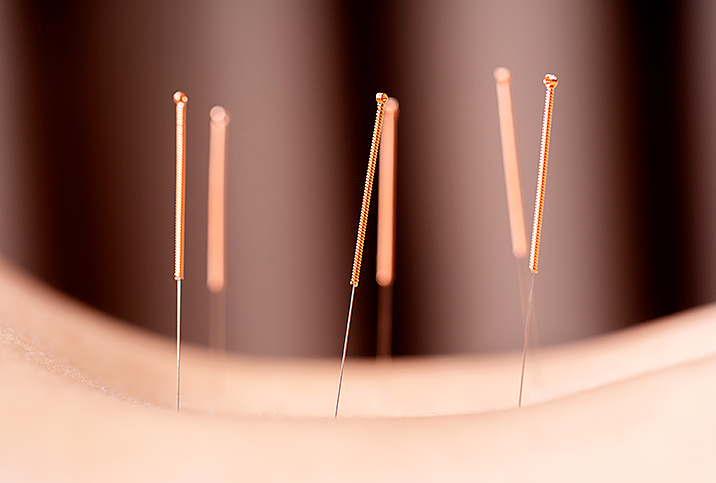
TENS devices are battery-operated and are about the size of a small cell phone. The Cleveland Clinic notes the electrode pads are placed in specific areas along nerve pathways, but acupuncturists might connect the TENS unit to acupuncture needles.
TENS isn't a new technology—it's been used to treat osteoarthritis, fibromyalgia, tendinitis, bursitis and diabetic neuropathy. But the use of TENS devices to treat period pain is a fairly new concept, which is why there isn't as much information out there on its efficacy in this area.
Studies on electronic devices for menstrual pain are promising
Gaither said there are many clinical studies, which evaluated quality of life and longevity of pain relief, that indicate TENS is a potentially useful treatment method. However, Gaither also noted that more conclusive studies are needed.
A 2020 overview of the available research on TENS for period pain management published in the International Journal of Women's Health noted the overall positive effects and potential value, but also discussed the limitations of the available studies, which were not uniform for recommended dose, duration or frequency of treatment.
"Variations...did not allow comparisons among protocols used in previous studies. The number of treatments ranged from one to several. The duration lasted from 20 minutes up to the continuous application for eight hours," the researchers explained.
A 2002 study, which was analyzed in the 2020 overview, found high-frequency (HF) TENS was effective in reducing menstrual pain. According to the authors of the overview, the 2002 study was updated in 2009, and since then, six new trials have been published supporting high-frequency TENS as an effective treatment for primary dysmenorrhea (PD).
The authors explained HF appears to be more effective among patients than low frequency (LF), stating, "HF TENS was shown to be more effective for pain relief than placebo TENS in PD patients. By contrast, LF TENS was as effective as placebo TENS or pill for pain relief."
The effectiveness of the device can depend on many factors, with each person experiencing a different result. It might not be a cure-all for someone with, say, endometriosis, but it could help alleviate pain while a more permanent treatment plan is being figured out.
Can anyone use TENS therapy?
There are companies that specialize in wearable, at-home-use electronic devices. These can be worn any time pain relief is needed, but seeking out the advice of a doctor is recommended before taking on this treatment at home.
Over-the-counter (OTC) TENS devices range in price and put out much less voltage than prescription units or those administered in a doctor's office. The price of OTC at-home TENS units can start as low as $20 for a simple product, and move upwards of $200 for something a little more in-depth and of higher quality.
If TENS treatments are considered medically necessary, insurance might cover the cost of having the treatment done in a medical facility. Depending on the insurance provider, an at-home unit could also be covered under an insurance policy if a doctor signs off on it and deems it medically necessary.
TENS therapy isn't for everyone, and some conditions do not allow for electrode pads to be placed in certain locations. Talk to your doctor first about proper placement if you have any of the following conditions:
- Pregnancy
- Implantable devices (such as a defibrillator or internal blood pressure monitors)
- Epilepsy
- Cancer
- Deep vein thrombosis
- Heart disease
Additionally, TENS should not be applied to broken or infected skin. Before undergoing any at-home TENS treatment, check with your provider for best practices.