Cervical Dysplasia Diagnosis & Treatment
Cervical dysplasia is a precancerous condition that can lead to cervical cancer if left untreated. Here's how early detection can dramatically reduce your chances of getting cervical cancer.
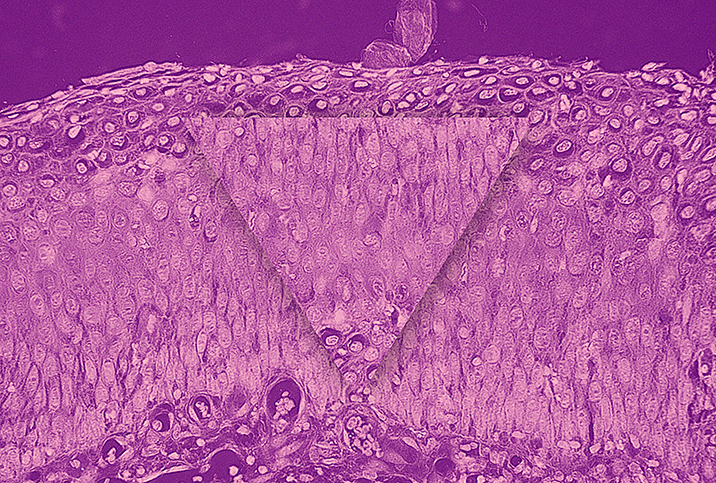
What is cervical dysplasia?
Cervical dysplasia, known as cervical intraepithelial neoplasia, describes the growth of abnormal cells on the cervix. Since these cells can become cancerous, many doctors consider cervical dysplasia to be the first stage of cervical cancer.
The human papillomavirus (HPV) is a sexually transmitted infection (STI) that causes cervical dysplasia. The immune system usually gets rid of HPV within eight to 24 months after exposure. However, some HPV infections, especially high-risk strains, remain persistent and lead to cervical dysplasia.
In the United States, between 250,000 and 1 million women are diagnosed with cervical dysplasia each year. Cervical dysplasia can occur in any sexually active woman but is most often detected in people between the ages of 25 and 35.
How is cervical dysplasia diagnosed?
Most cervical dysplasia cases don't include noticeable symptoms. A routine Pap smear (or Pap test) typically finds abnormal cells. During a Pap smear, the doctor accesses the cervix by inserting a speculum into the vagina. Next, a swab collects cells on the cervix. Cell samples are sent to the lab for screening. In addition to checking for abnormal cells, testing for high-risk HPV strains commonly associated with cervical cancer can help determine your risk.
For HPV-positive patients or people with abnormal cells, the next step is a colposcopy, where the doctor uses a speculum and applies liquid, often acetic acid, to the cervix to make any abnormalities more visible.
Next, the doctor uses a colposcope, a specialized magnifying device, to examine the cervix. The colposcope stays outside the body during the exam. Suspicious cells are biopsied and sent for further testing. For most people, a colposcopy involves the same level of discomfort as a Pap smear. However, a biopsy can lead to mild cramping, pain or light bleeding.
How is cervical dysplasia treated?
Treatment for cervical dysplasia depends on the severity. Milder cases don't require treatment and often resolve with time. A repeat Pap smear after one year or more, often depending on the doctor's recommendation, along with an HPV test will allow your doctor to monitor any changes.
Abnormal tissue should be removed if cervical dysplasia is severe. Ablative procedures can destroy the affected tissue with cryotherapy or laser therapy. However, surgical removal through excision is generally preferred. Surgical removal preserves the cells so they can be tested. Excision also reduces cervical dysplasia's rate of recurrence. It is important to determine whether all the precancerous cells were removed by making sure the margins of the biopsy were clear.
There are two main types of excisional procedures:
- Loop electrosurgical excision procedure (LEEP): A thin, heated and electrically charged wire loop removes the affected cervical tissue under local anesthesia in your doctor's office.
- Cold knife cone biopsy: For more severe cases, you'll be given general anesthesia or spinal or epidural anesthesia, which numbs you below the waist. A scalpel or laser removes the affected area of dysplasia.
A cold knife cone biopsy usually produces a better tissue sample than the LEEP because it's more precise and can remove more tissue.
A follow-up Pap smear is recommended within one year or less after surgery, even if the dysplasia was removed entirely. If your follow-up finds cancer or dysplasia, you can be referred for prompt treatment. As with all forms of cancer, early screening and detection offer the best chance for a favorable outcome.


















