Treatments for Advanced Penile Cancer Are Few but Getting Better
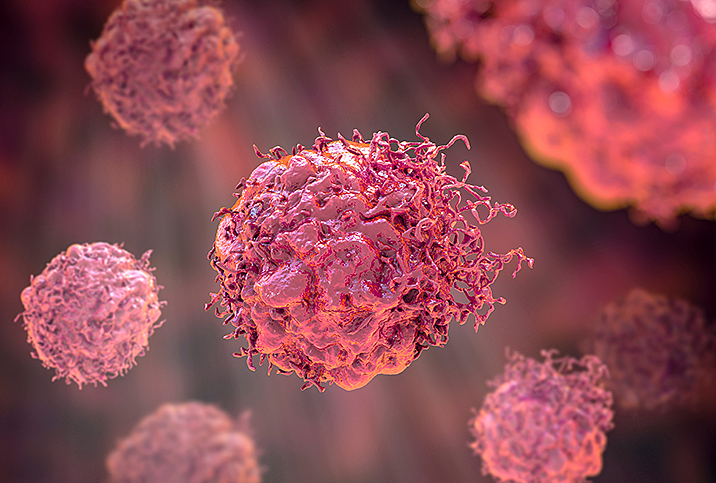
When a condition such as cancer has the potential to cause widespread damage to multiple interconnected systems within the body as it spreads and grows, it can be difficult to say where problems begin and end.
Penile cancer is a particularly rare form of the disease, and this fact is partially responsible for the lack of viable options for treatment. Advanced penile cancer can refer to a few different aspects within the larger frameworks of both urological and general oncological care, according to Nirmish Singla, M.D., M.Sc., a urologic oncologist at the Brady Urological Institute at Johns Hopkins Medicine in Baltimore.
Explaining advanced penile cancer
"You could view the word 'advanced' in a few different ways," Singla said. "There's advanced in the sense of the end of the spectrum, where you're talking about metastatic disease and basically the cat's out of the bag, and essentially the cancer has spread to other parts of the body."
Penile cancer is often addressed once the cancer has established metastatic growth, which means other parts of the body may be prioritized over genitalia when considering the grand scheme of saving lives and preserving quality of life.
"When we think about penile cancer, there's sort of a local setting where it's just in the penis alone and not anywhere else, and then there's a locally advanced setting where it's starting to get into the more advanced local stage and still may not have spread elsewhere," Singla said. "In terms of how we, as clinicians, approach penile cancer, it's very much multidisciplinary."
Urologists often work very closely and collaboratively with oncology colleagues across a spectrum of expertise. Additionally, depending on the treatment route and the general nature of the cancerous spread, it may be necessary for radiologists or other specialists to become involved in the process of evaluating options and weighing the consequences of each one.
'It is a fine balance that we have to tread between what is a quality-of-life motivation and what can we offer from the standpoint of cancer control.'
Surgery is the traditional mainstay for treating primary tumors in the penis. This might include a total or partial penectomy—the removal of all or some of the penis. Surgery can provide important information about the tumor and the cancer itself to direct the next step in treatment, which is trying to address or prevent the cancer's spread.
If the cancer has already advanced, the focus may have to be on the palliation of symptoms and easing the burden for the patient—providing comfort and some improvement in quality of life—rather than focusing on managing the cancer's development.
Singla said clinicians have to navigate carefully when treating metastatic disease. Patients are likely to be experiencing a range of mild to severe symptoms, and the wrong decision runs the risk of worsening the suffering or decreasing the chance of relief for the patient.
"It is a fine balance that we have to tread between what is a quality-of-life motivation and what can we offer from the standpoint of cancer control," he said.
He said doctors have to determine whether treatments are going to do more harm than good for a patient's longevity, durability and comfort.
Penile cancer risk factors
The big question surrounding cancer is what can be done to avoid exposure to potentially cancer-causing elements. Risk factors for cancer development can be tricky to determine in many areas, but with penile cancer, some of the trackable considerations might surprise you.
"The most common risk factor for developing penile cancer is actually a lack of neonatal circumcision," Singla said. "It tends to be one of the common risk factors associated with the subsequent development of penile cancer later in life [and] to be a disease that affects the elderly population rather than the younger population on the whole.
"Things like chronic inflammation, sometimes tobacco use, poor hygiene, sexually transmitted diseases and certain conditions—lichen sclerosus or balanitis, sometimes even penile trauma—those are the types of risk factors that may lead to the development of penile cancer," he said.
Early diagnosis is essential
As with many health issues, men may be reticent to acknowledge problems in the genitalia department and be reluctant to express concerns about penile cancer to their doctor.
Singla said this is an important obstacle to overcome if individuals want to prevent significant suffering that might result from a penile cancer diagnosis.
"In terms of timely diagnosis, it tends to be a relatively rare cancer overall, but the important things to be cognizant of is if one were to notice some difference, some sort of new lesion or some area of spontaneous bleeding, sometimes an ulcer around the penis, and that can be anywhere on the glans part of the penis or just on the skin of the penis itself," Singla said.
Making these observations and promptly following up with a healthcare provider can be the difference between potentially severe and less severe consequences from treatment, he added.
"If there are any of those [symptoms], or even just a palpable, hard nodule, these are the types of ways that penile cancer can sometimes present initially," he said. "And so, ideally, the ability to kind of catch it early has a greater chance of improving the overall outcome from the cancer-control perspective, and so that is really important for timely diagnosis."
In this regard, the onus is on the patient to be proactive and responsible for cleaning the penis as well as reporting changes to a primary care doctor or urological care team. Singla said uncircumcised men should make extra effort to retract the foreskin and clean the penis thoroughly, which also provides an opportunity for self-examination. It's important to keep an eye out for cold sores and other unusual changes to the surface of the penis and to report them to your doctor.
Your urologist and general healthcare team want to help. Men who have a good rapport with their urologist may find it unsettling to have to incorporate appointments and exams with new, unfamiliar physicians. But this handoff is an important part of the care process any time cancer is diagnosed, according to Matthew Mutter, M.D., a urologist in the New Orleans area.
"From a general urology standpoint, if I have/diagnose a patient with penile cancer, I will refer them to my urologic oncologist partner for further management," he said. "At that point, the urologic oncologist will work with radiology, specifically IR [interventional radiology], for discussion of biopsy of suspicious lymph nodes."
This collaborative effort on the part of doctors and radiologists with various disciplines provides optimism about penile cancer treatment options of the future.
A future for penile cancer treatment
Obviously, a partial or complete penectomy is not an ideal outcome for anybody dealing with symptoms that affect the penis. But it's important to recognize that this level of intervention can save lives and prevent the condition from worsening.
Fortunately, progress is being made with penile cancer treatment options and surgical intervention, according to Singla.
"More and more, we've had an interest in trying to do penile-sparing approaches, meaning that you just remove the cancer within an appropriate margin and spare the penis," he said. "From the standpoint of quality of life and functionality, I think patients certainly appreciate that more."
Doctors stress the importance of early intervention, because while penis-sparing procedures are available, they're more likely to be used on patients whose cancer has been detected earlier rather than later, Singla said.