Substance Abuse & Addiction: Myths & Misconceptions

Substance abuse and addiction are serious problems in the United States; in fact, about 21 million people fight at least one addiction. Since 1990, deaths from overdoses have more than tripled, costing the American economy $600 billion a year.
Misinformation contributes to the widespread issue of substance abuse and addiction. To set the record straight, here is the truth to counter some of the most common myths about substance abuse and addiction.
Myth: Substance abuse and addiction are a choice.
Reality: Many substance abusers and people who develop an addiction begin as recreational users. But over time, substances create a chemical imbalance in the brain, leading to addiction, particularly for people with a genetic disposition. As a result, addiction is not a choice. It's a disease where the body and brain become dependent on a substance due to significant, often debilitating, withdrawal symptoms if deprived of it. The chemical imbalance is related to the rewiring of the dopamine receptor pathway due to the flooding of receptors over time, leading to impulsive behavior and dependence on drugs or alcohol with even small quantities of consumption.
Myth: Addiction and substance abuse are synonyms.
Reality: Despite the interchangeable use of "addiction" and "substance abuse" by most people outside the medical and treatment community, the terms are inherently different.
Substance abuse is a pathway to full-blown addiction. People who are able to identify substance abuse before it becomes an addiction are often more successful at kicking the habit than those with addiction, thus avoiding consequences that may be irreparable.
Substance abuse refers to the use of drugs and alcohol to the detriment of the user, possibly including legal problems, hurting others or failing to meet obligations with family, school or work.
Addiction may include symptoms of substance abuse, but it becomes even more harmful to the user. For example, a user:
-
Experiences physical and psychological withdrawal symptoms just hours after the consumption of a substance.
-
Lives a lifestyle that revolves solely around achieving a high.
-
Goes back to drugs or alcohol despite near-death experiences or hospitalization.
-
Commits crimes to fuel drug use or obtain funds illegally to purchase drugs.
-
Makes numerous attempts to quit with no success, even with treatment.
-
Undergoes a withdrawal from passions, hobbies, family and friends.
Myth: Only voluntary treatments for substance abuse and addiction are effective.
Reality:In many facets of life, the willpower and desire to change are catalysts to success. Substance abuse and addiction are a different story. Since substances can cause chemical rewiring of the brain, a vast majority of users are either in denial or don't want to undergo treatment.
Due to these feelings, often beyond their control, substance abusers and people with addiction issues will resist help and are far less likely to seek treatment on their own. Often, high-pressure tactics—typically court-ordered treatment or interventions from friends and family—are the only effective ways to help these individuals to get better.
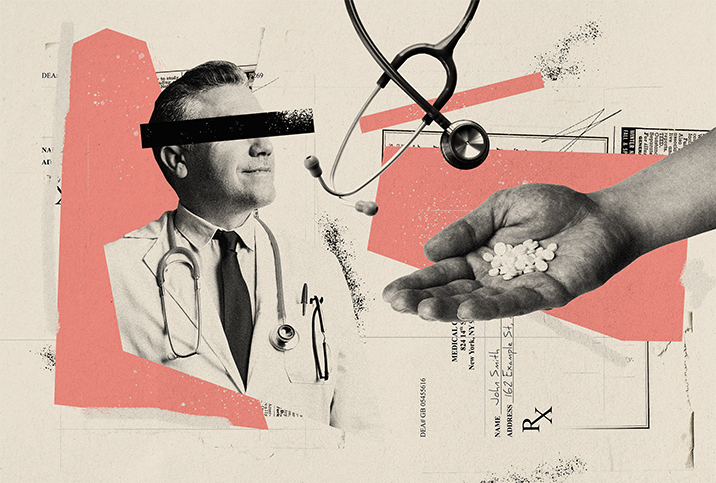
Myth: Substance abuse and addiction are lower-class problems.
Reality: Anyone can develop substance abuse issues or addiction. There is growing evidence of a strong genetic link to drug and alcohol abuse, addiction and dependence. The ease of obtaining substances and the quality of the substances are also factors in abuse. Even people who had no intention of doing drugs—for example, patients who take prescription pain medication—can develop substance abuse issues or addiction problems. People often mix medications, illegal drugs and alcohol, adding to the complexity of the problem.
The crack epidemic of the 1980s and 1990s mainly affected lower-class, urban, Black neighborhoods, fueling a view that drug use and low socioeconomic status were tied together. The opioid crisis of the 2000s and 2010s—opioids, stimulants and methamphetamines, really—debunked that myth, to some degree, by permeating nearly every socioeconomic level and racial group in America.
Myth: Pharmaceutical treatments aren't effective for substance abusers and people with addiction.
Reality: The use of pharmaceutical products to treat substance abuse and addiction has been around since the Food and Drug Administration's approval of methadone in the 1970s. However, an abstinence-based approach to drug abuse treatment was the more accepted method in the rehabilitation community.
But in the past decade, pharmaceutical companies have developed more efficient drugs to treat patients. Buprenorphine has become more popular in rehab centers, while physicians continue to prescribe methadone. Compared to abstinence, these prescriptions have shown marked improvement in treating patients, and when combined with abstinence strategies and social support/programs, they can be even more effective.
If you suspect that you, a friend or a family member are suffering from substance abuse or addiction, time is of the essence. The earlier a person seeks treatment, the greater the chance they overcome this debilitating disease. Relapses are common, and it's important for individuals to have family, social support and programs to help keep them on track.
For more information or free advice, contact the Substance Abuse and Mental Health Services Administration or call its national helpline at 1-800-662-HELP (4357).
Myth: Prescribed narcotics must be safe.
Reality: Narcotics—even prescribed ones—aren't always safe. Over time, a body grows more tolerant and the current dosage becomes ineffective at alleviating pain. Many doctors will then prescribe higher doses. If the patient then starts to self-administer the drug, the dependence grows to the point of abuse or even addiction.
Because of the potential for abuse, you should understand your family history of addiction before you begin a prescription narcotic regimen.
Myth: If I maintain a job and relationships during narcotic use, I am not addicted or abusing it.
Reality: Just as a functional alcoholic fulfills obligations, looks healthy and goes to work, a person who abuses or is addicted to narcotics can act similarly. That doesn't mean, however, that such narcotic use is without issues. It may take months or even years for functional use to lead to a diagnosis of addiction, but the chance of abuse lingers nonetheless.
Denial and increased tolerance are two hallmarks of a functional narcotics user, and the inward perception that nothing is wrong can hinder treatment possibilities. If you or a person you know consistently uses narcotics, it may be a sign of potential abuse.