RPLND Offers a Robotic Alternative to Open Testicular Cancer Surgery
In 2018, Ben Walborn, a then-37-year-old airline pilot and Navy reservist, was on vacation with his family in Florida when he made a startling discovery. During a shower, he noticed his right testicle was double the size of the left one.
He promptly went to the Navy hospital in Pensacola, where personnel performed an ultrasound.
"They're like, 'We want to remove it,'" Walborn said. "I'm like, 'No, I'm on vacation and I don't even live here.' They said, 'I suggest you cut your vacation short, go home and see the first urologist who will see you.'"
So that's what Walborn did.
The urologist looked at the ultrasound and said he needed to remove the right testicle that night. Walborn underwent an orchiectomy, the term for the outpatient surgery that removes the testicle.
Prior to the orchiectomy, blood tests indicated Walborn had an elevated alpha-fetoprotein (AFP), a tumor marker, of 855 nanograms per milliliter (ng/mL). About a month after the surgery, his level decreased to 4 ng/mL, which is within the range of a healthy adult. Four months later, Walborn had his first postsurgical CT scan, which showed that two of his retroperitoneal lymph nodes were enlarged.
At that point, Walborn reached out to Phillip Pierorazio, M.D., one of the few urologists in the country who regularly performs robotic retroperitoneal lymph node dissection (RPLND), a surgery that uses the help of a robot to remove the lymph nodes in the back of the abdomen.
Walborn elected to undergo RPLND instead of chemotherapy, which, while highly curative for testicular cancer, carries long-term side effects and toxicities.
In May 2019, Pierorazio performed the robotic RPLND on Walborn using a state-of-the-art device with a robotic main arm and a support arm, meaning he had to make only two small incisions.
"He said, 'The less I can put in you, the better, and the faster the recovery,'" Walborn said. "I was a big fan of that. He put me at ease."
Pierorazio removed 22 retroperitoneal lymph nodes, 10 of which had small traces of embryonal carcinoma, a type of nonseminoma testicular cancer. The surgery was a success, and more than three years later, Walborn remains cancer-free.
What does RPLND surgery entail?
RPLND is a mainstay treatment option for stage I and II nonseminomatous germ cell tumors (NSGCT). Nonseminoma is generally more aggressive than seminoma, the other main type of testicular cancer.
"For men who have cancer that has spread from the testicle to lymph nodes, surgery can be curative and offer them a chance to avoid chemotherapy," Pierorazio explained.
Further, some forms of testicular cancer are not responsive to chemotherapy, so they have to be surgically removed regardless.
The vast majority of patients who have early-stage NSGCT are cured by RPLND, according to Pierorazio.
"The home run is small-volume cancer found in the lymph nodes; no need for chemotherapy, and basically cured two years later," he said.
This robot-assisted method has come about only in the past 10 to 15 years.
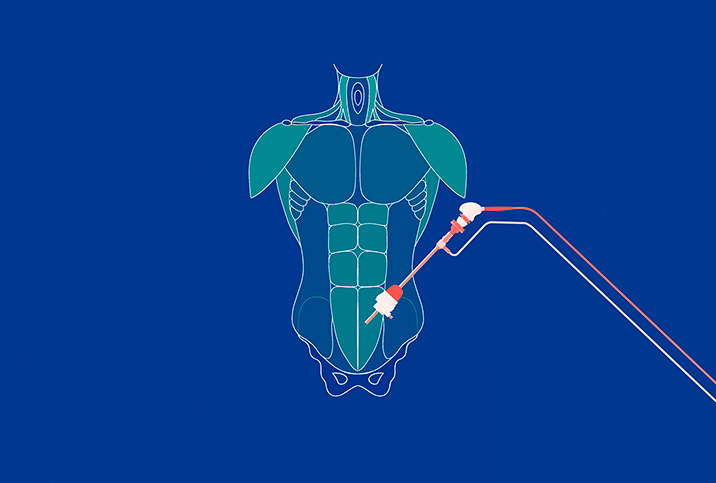
RPLND has traditionally been performed through a large midline incision from the xiphoid (the bone at the bottom of the chest) to the pubic bone (the bone at the top of the pelvis).
"You have to move all the abdominal organs out of the way to be able to get to the area that's called the retroperitoneum, which is basically surrounding the aorta, vena cava and the blood vessels that go to the kidneys," Pierorazio explained.
Robotic RPLND is the same surgery, but instead of one large incision, it's typically done through four or five incisions measuring 8 millimeters to 1 centimeter. This robot-assisted method has come about only in the past 10 to 15 years and has yet to be included as a standard option in the American Urological Association (AUA) guidelines. However, high-volume cancer centers have been using robotics more in recent years for select patients.
Samuel Haywood, M.D., a urologic oncologist at Cleveland Clinic, said the center has done a number of robotic RPLNDs with positive results.
"I think it's pretty likely people will do more and more robotic RPLNDs, and it's our duty to try to figure out ways to do that safely," Haywood said.
Advantages of robotic over open surgery
The main distinction between traditional open surgery and robotic RPLND is in recovery times, Pierorazio explained.
The traditional open surgery consists of two to four hours in the operating room, three to five days in the hospital, and four to six weeks of physical recovery. Long-term recovery is three to six months, which is about the same as with robotic surgery.
But short-term recovery rates tend to be faster with a robotic procedure. Most men are back to work, fully recovered, within two to three weeks rather than four to six, Pierorazio said.
He explained it generally takes three to five hours to complete robotic surgery. Complication rates are similar for the two procedures.
"We just don't have long-term robot data yet just because it's a relatively new approach," he said. "Once you hit three to six months and beyond, the outcomes are pretty similar. The advantages are in the short term."
Most men are back to work, fully recovered, within two to three weeks rather than four to six.
Another advantage of robotic surgery is it's more cosmetically appealing.
"You don't have this big incision down the middle of the body; you've got these small keyhole incisions that are often easier to hide," Pierorazio said.
Pierorazio does not recommend a robotic RPLND if the patient has had chemotherapy.
"My personal belief is that we should learn to walk before we run, and we really should be proving that robotic RPLND is safe and reasonable in the primary setting first," he explained. "We haven't really proven that yet. That's why I continue to call it investigational. In select patients in the post-chemotherapy setting, a robotic RPLND is reasonable, but I think it's much harder to select those patients."
Side effects and complications of RPLND
For both open surgery and robotic RPLND, potential side effects include injury to blood vessels, such as bleeding, pain and infection. Patients may experience a leak of the lymphatic vessels that go to the lymph nodes.
The surgery can also cause scar tissue, which can lead to bowel obstructions. Some men may experience a loss of ejaculatory function because the nerves that control ejaculation run in the retroperitoneal area.
"In order to combat that, we try to do a nerve-sparing procedure," Haywood said. "[W]e're able to save ejaculation in 90 to 95 percent of patients."
Walborn said his biggest fear going into his robotic RPLND was whether he'd be able to have intercourse afterward. Pierorazio told him some of his lymph nodes were tangled among the nerves. During the surgery, Pierorazio cut two of the three nerves responsible for ejaculatory function. He told Walborn that he couldn't say if he'd be able to ejaculate again, but he would have orgasms.
"He said, 'You will still have all the functionality and feel, you just won't have the mess,'" Walborn said with a laugh. "Well, that's perfect. That's like the best of all worlds."
In the first month after RPLND, Walborn couldn't ejaculate at all. Eventually, semen started to emerge.
"It does seem, even to this day, that it's at a lesser amount, but that's not a big deal," Walborn said. "I have full functionality."
He and his wife, now both in their 40s, have sex multiple times a week.
"We still have two kids and we're busy," Walborn said. "That's usually when a lot of my friends are saying they're having sex once a month. We're still very happy and very well engaged."