What Peritoneal Dialysis Can Do for You

If you have chronic kidney disease (CKD), your kidneys are unable to clean blood as well as they should, resulting in toxic waste buildup in the body that can lead to increased blood pressure, heart disease, stroke and death. It's estimated there are about 37 million Americans suffering from chronic kidney disease, with as many as 9 in 10 adults unaware they have the condition.
If you've been diagnosed with kidney disease, you may feel like it's only a matter of time before you end up on the donor list. However, with early intervention, a clear health plan and innovations in dialysis, your chances of kidney failure could be greatly reduced.
"The truth is that only 5 percent of kidney patients will ever experience kidney failure," said Holly Kramer, M.D., M.P.H., professor of public health sciences and nephrology, and immediate past president of the National Kidney Foundation Board.
What is peritoneal dialysis?
The most well-known form of dialysis is hemodialysis, in which the patient's blood is filtered to remove waste materials in place of the kidneys. This process is more invasive because the patient must undergo a series of procedures to access the main artery, set up a port and wait for the tissues surrounding the port to properly heal before dialysis can begin, which, according to Kramer, can sometimes take six weeks.
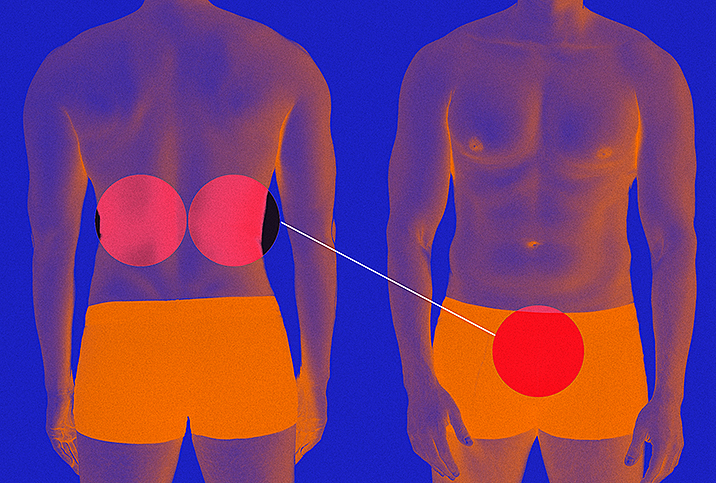
Peritoneal dialysis, however, is the process of removing waste from your body through your abdomen in place of, or in conjunction with, your regular kidney function. This treatment allows patients to perform their dialysis at home without disrupting their daily lifestyle. Peritoneal dialysis devices are so portable that patients who wish to travel can treat themselves in their hotel room.
Peritoneal dialysis is growing in popularity because the preparation for dialysis is much shorter than hemodialysis. The procedure to set up the port is minimally invasive, as the port is inserted into the abdomen through the navel. Once the port heals, typically in two weeks, the patient will attach their port to specific solutions that will fill the abdomen, filter out the toxins and then be drained by the patient.
The process typically takes about four hours each day; many patients will perform the process overnight for maximum convenience. Most patients can continue playing sports and other high-intensity activities without the risk of damaging the device.
The factors that lead to dialysis
"One of the many misconceptions that I frequently address is that kidney disease rarely results in dialysis," said Susan Quaggin, M.D., F.A.S.N., and president-elect of the American Society of Nephrology.
"Once a patient is diagnosed with kidney disease, they should seek a consultation with a nephrologist, regardless of the stage of their disease," Kramer explained. "Once a patient's kidney function is less than 20 percent, we begin the process of dialysis, but we seek to inform the patient early on so they have time to decide what form of dialysis is best for their lifestyle."
Both Kramer and Quaggin emphasized that kidney disease can most often be treated by your primary care physician with medicine, and may never advance beyond this routine maintenance. However, meeting with a nephrologist and a nurse educator soon after your diagnosis can ensure you have a team in place if your disease does progress.
"Every patient is different, and we want to consider each patient's risk factors, including lifestyle and diet, heredity and other diseases that might increase the risk of kidney disease progression," Kramer clarified.
"Testing your kidney function can be performed via a blood test or urinalysis," Kramer added. "While these tests are not part of a routine blood panel, they are covered by insurance, and we recommend that every patient requests this test as part of their annual physical."
At-home and outpatient dialysis
Part of the early planning stage of a kidney diagnosis is ensuring patients fully understand what led to their diagnosis and how they can prevent or slow progression. During this stage, physicians can assess the factors that may help a patient decide which method of dialysis will work best for them.
When a patient chooses outpatient dialysis, they are choosing to spend four hours three times a week in a hospital, where a nurse will perform dialysis. In an at-home setting, patients will perform the task themselves. While the process itself is relatively simple, there are other factors that can complicate a patient's ability to manage their own care.
"Most at-home considerations should take into account the patient's support system, because an extra set of hands in the managing of materials will help the patient be successful in this process," Kramer explained.
One of the hardest aspects of the process is the handling and storage of the solutions that perform waste extraction. Kramer noted the solutions for one treatment can be large and patients will typically receive even larger boxes of these solutions at one time. Needless to say, these supplies can be heavy and cumbersome, so the help of a family member can be important for elderly patients or patients who might have physical impairments that limit mobility. Patients must also have the space to store these materials and solutions somewhere safe and secure in their home.
In addition to the solutions, patients must clean their ports and change tubing and other supplies related to their treatment to prevent infections.
Self-advocacy and education
Being diagnosed with any chronic illness can be scary. Kidney disease can be especially frightening because of the misconceptions surrounding treatment and patient prognosis. The trick is to learn as much about the condition as you can, ask questions of your healthcare providers and listen carefully to what they say.
As more people are diagnosed with kidney disease each year, researchers are working harder than ever to create more effective medications and accessible dialysis treatments that can better ensure a long and healthy life.