What to Know About Perineum Tearing During Childbirth

Every birth is unique and when it comes to vaginal deliveries, there are more variations than you might imagine—from the woman's position to the baby's orientation to how long it takes to deliver and more.
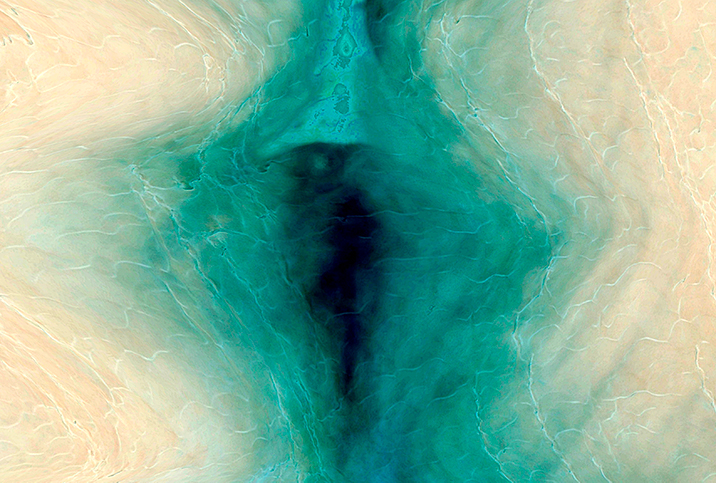
There is one thing they all have in common, though: a very large (relatively speaking) head must come through a very small opening. This is when the woman's perineum, the skin and muscle between the vagina and the anus, can get torn.
According to the American College of Obstetricians and Gynecologists (ACOG), an estimated 53 percent to 79 percent of vaginal deliveries result in perineal tearing.
There are ways to reduce the likelihood and severity of perineal tears. If they do occur, the right treatment and care will play a big role in the nature and length of recovery.
What increases the risk of perineum tearing?
We asked the director of perinatal services at NYC Health + Hospitals/Lincoln in the Bronx, Kecia Gaither, M.D., F.A.C.O.G., who is double board-certified in OB-GYN and Maternal-Fetal Medicine, if there is a way to predict whether perineum tearing is likely to occur.
"A short perineum may raise suspicion," Gaither said. "One can have a 'guesstimate'; however, until the baby's head is crowning, uncertainty exists."
In addition to a short perineum, other factors are somewhat predictive. "It's really a combination of mother and baby that determines if a tear is going to occur," said Nanette Santoro, M.D., an OB-GYN at the University of Colorado Hospital.
"If her baby is large and if she is small, she is at higher risk for a tear," Santoro continued. "In particular, the baby's head size and orientation as it comes through the vagina at birth will put her at more or less risk."
'It's really a combination of mother and baby that determines if a tear is going to occur.'
Santoro explained that "most babies' heads tilt forward a bit and the back of the head is on top at delivery (as if the baby is looking down at the floor when the mother is on her back). Babies whose heads come out in the opposite direction [facing up] require more width from the vagina, which puts a woman at risk."
Additionally, "the pace of the delivery can also be a risk factor," Santoro said. "A very fast second stage of labor [which begins when the cervix is completely dilated] will force that baby's head out before the perineum has had time to stretch."
There may also be "some genetic or endogenous factors, like a woman's connective tissue quality, that put her at more or less risk," Santoro concluded.
However, Santoro cautioned that the above risk factors come with a caveat: "All of these risk factors are weak. When we review cases of patients who have tears and review their management, sometimes they are present and sometimes they are not."
Other risk factors include:
- If a woman is giving birth for the first time, if she's having a vaginal birth after a cesarean section or if she's age 20 or younger.
- When the baby weighs more than about 9 pounds, has a head circumference exceeding 14 inches, is born face-up or if a shoulder gets stuck behind the mother's pubic bone during birth.
- When delivery involves instruments, such as forceps or a vacuum; the second stage of labor lasts more than an hour; when the woman is given an epidural, oxytocin or a midline episiotomy; or when the woman delivers in lithotomy position (her legs are higher than the hips) or deep squatting position.
Types and treatment for perineal tears
If you do experience a perineal tear, first, there will be bleeding. Most of the time, bleeding can be quickly controlled with pressure, although it might require surgical repair.
Tears are classified into four different types, depending on the severity:
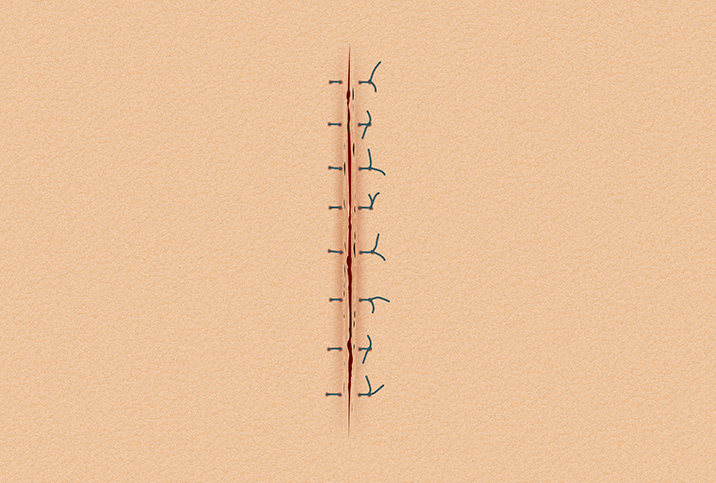
- First-degree tears: These are small and superficial, and usually heal within a few weeks without treatment.
- Second-degree tears: Affecting the skin and muscle, these usually require stitches, which will dissolve in a week or two.
- Third-degree tears: Superficial or deep injury to the external anal sphincter.
- Fourth-degree tears: Extend completely through the sphincter and the rectal mucosa.
Third- and fourth-degree tears have to be repaired surgically, and usually take about three months to heal.
How to ease your recovery from perineal tearing
Recovery from perineal tears can be uncomfortable or quite painful, depending on the number, depth and length of the tears. You can generally expect at least a week of pain that affects sitting, walking, urinating and bowel movements.
The University of Michigan Health offers the following recommendations for reducing pain and promoting healing:
- Try keeping an ice pack on the area.
- Take sitz baths (sitting in a tub of shallow, warm water).
- Take pain medicine as directed.
- Take stool softeners and drink lots of fluids to ease bowel movements.
- Keep clean but do it gently. Clean the area using warm water from a squeeze bottle and pat it dry with gauze or a sanitary wipe.
Can anything decrease the risk of perineum tearing?
According to researchers, warm compresses and perineal massage are the only interventions shown to decrease the frequency of severe (third- and fourth-degree) tearing.
Gaither explained that perineal massage increases "elasticity to the tissues, hopefully to allow stretching over the baby's head without tearing."
She said the massage also lowers the risk of tearing, assists those women who have had an episiotomy or other procedure by gently stretching the scar tissue and increasing blood flow to the area. If there is a need for an episiotomy, massage can decrease "the number of stitches needed by decreasing the depth of cutting needed."
The position the mother is in during delivery also matters. According to researchers, approximately 68 percent of women who give birth vaginally in U.S. hospitals do so lying on their back and about 23 percent give birth in a semi-reclining, upright position, even though these positions have "distinct disadvantages with no demonstrable benefits to either mother or infant."
A 2019 review and comparison of common maternal positions during the second stage of labor published in the International Journal of Nursing Sciences stated that positions where the woman is lying on her back, flat and facing up (supine) or with legs raised (lithotomy position) should be avoided "for the possible increased risk of severe perineal trauma, comparatively longer labor, greater pain, and more fetal heart rate patterns."
The review found that upright and lateral positions "may have more potential benefits in improving maternal and neonatal outcomes and dealing with certain obstetric complications."
Recovery is in your future
While perineal tears are not inevitable in every vaginal birth, they are very common and most of the time will heal on their own. Whether your tears are minor or require surgical intervention, follow your doctor's advice (which may include the simple care tips above) and you'll be on the road to recovery.