Imaging Tests Play a Significant Role in Detecting Testicular Cancer
In society today, everyone should know testicular cancer is one of the most curable forms of the disease. In fact, this truth is why men and boys are encouraged to check their testicles early and often. If you detect it soon enough, testicular cancer has a 99 percent five-year relative survival rate, according to the American Cancer Society.
But there's more to diagnosing a man with testicular cancer than doing the old post-shower "roll 'n' feel" test for lumps.
If you or your doctor find something, here's how imaging and other tests can help determine what's going on down there.
Act on any anomaly
First, don't panic.
It's important to remember a lump can appear on a testicle for a variety of reasons. Testicular cancer is rare—it affects only about 9,400 men and boys each year in the United States—and all kinds of weird things can appear in the scrotum.
However, it's crucial that you get any anomaly checked.
"Typically, this starts with the guy [or someone else] noticing a hard lump within the testicle," said William O. Brant, M.D., a urologist with Summit Urology Group and chief of urology at the Salt Lake City Veterans Affairs Medical Center. "This is why self-exam—usually in the shower—is so important. Usually, the first imaging is an ultrasound of the scrotum, which is very good for looking for testicular tumors."
Ultrasound
The ultrasound device is a wand-like instrument that uses high-frequency sound waves to create images from inside the body. If you've ever seen proud parents-to-be hold aloft a grainy picture of their developing offspring in the womb, that's an ultrasound image, known as a sonogram.
Ultrasounds for testicular cancer are noninvasive and completely painless, and don't expose you to radiation or require any special preparation on your part.
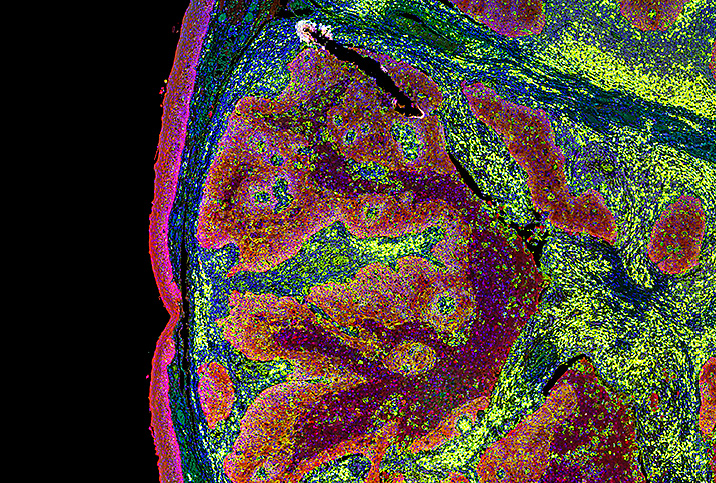
"If there's anything we feel is abnormal on a [physical] exam, we always get an ultrasound to confirm," said Amy Pearlman, M.D., a urologist and the director of the men's health program at the University of Iowa. "We're looking for what does the testicular tissue look like—you can pretty easily see a mass."
The ultrasound is also a useful tool for seeing what's hidden inside the testicle.
When someone can feel a lump, it's because a cancerous mass extends outward from the smooth edges of the testicle. But sometimes a tumor may be mostly hidden inside the testicle—or obscured in another way.
"You can't always feel the entire mass on the testicle," Pearlman said. "If someone has some testicular swelling or a hydrocele, you won't be able to actually feel the testicle itself. You can have lumps that occur inside the testicle that you can't feel with your hand. So the ultrasound will show us."
The ultrasound is also great at helping doctors differentiate noncancerous lumps—for instance, those that frequently appear in the epididymis, the tightly coiled tube that sits just behind the testicle.
"It's very common to have cysts or lumps in the epididymis, but that is very rarely cancer," Pearlman said. "But sometimes, you can't tell between that and the testicle [manually]. So we'll always get an ultrasound in those cases."
Blood tumor markers
After the ultrasound, you'll likely get a blood draw to look at what are called tumor markers. These blood tests help confirm if a lump is likely to be cancerous and what kind of cancer it might be.
"Even if someone's blood markers are negative, if they have a mass in their testicle that looks suspicious on ultrasound, we're going to remove that mass," Pearlman said. "A mass in a testicle is pretty much assumed to be testicular cancer until proven otherwise. But that testicle usually comes out."
CT scans
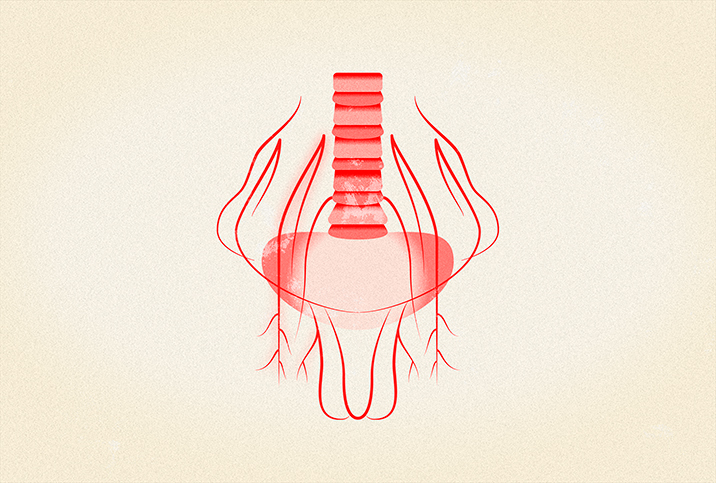
Once the testicle is removed by orchiectomy, it's examined by a pathologist to determine whether the lump was cancerous and what kind of cancer it is.
Depending on those results, your doctor may recommend a computed tomography (CT) scan, formerly referred to as a computed axial tomography (CAT) scan. This is a series of X-rays of your abdomen, chest and pelvis from various angles to determine if the cancer has spread.
"[Depending] on what the pathology comes back as once the testicle is removed, in terms of the depth of invasion and the type of cancer it is and the tumor markers, if they were elevated or not elevated before surgery—and we're checking tumor markers after surgery, as well—depending on all of that information, then patients may or may not need follow-up CT scans and bloodwork," Pearlman said.
Other imaging
As well-known and reliable as CT scans are, they are not the only imaging tool at doctors' disposal.
Magnetic resonance imaging (MRI)
Another common imaging tool is magnetic resonance imaging, or MRI. The patient lies in a large, tube-like structure while enormous magnets are used to create an image of the body's interior. However, MRI is rarely used in initially diagnosing testicular cancer. The American Urological Association guidelines specifically recommend against using it in routine testicular cancer diagnosis.
The only exception is when the patient is allergic to the contrast materials injected during a CT scan or if the patient has kidney issues, as this contrast dye can further stress already weakened kidneys.
X-ray, PET scan, bone scan
Imaging tools such as X-rays, positron emission tomography (PET) and bone scans are rarely used for the initial diagnosis of testicular cancer. However, if your post-orchiectomy blood markers remain elevated, your clinician may order one or more of these scans to check if cancer has spread to your chest, lymph nodes or bones, respectively.
If the cancer is suspected to have spread to the brain or spine, your doctor might order an MRI of those areas, as well.
Positive outcomes
Finding a lump on a testicle is a scary situation. Luckily, there are double- and triple-checks to ensure if it's cancerous before drastic measures are taken. Plus, with the aid of modern imaging tools, testicular cancer—even if it has spread—remains a highly survivable disease.
"Testicular cancer, in general, has a very high cure rate," Pearlman said. "That's the important part: Men need to know about their bodies. They need to start feeling their body parts early on, so if they realize there are changes, they need to go to a healthcare provider so they can at least get reassurance or so they can be taken care of."