How to Cope With Cystoprostatectomy

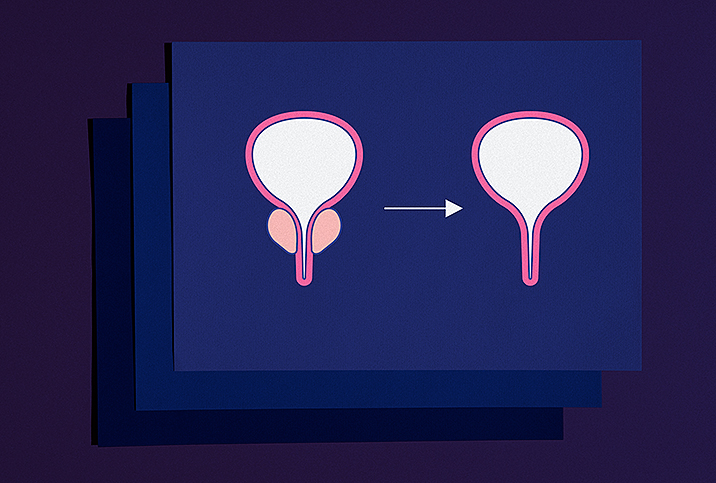
Men suffering from an aggressive form of bladder cancer may need to undergo surgery to remove their entire bladder and prostate gland. Called cystoprostatectomy, this surgery is a combination of a cystectomy (removal of the bladder) and a prostatectomy (removal of the prostate).
"The reason why they're usually removed together is because they're intimately involved; they're connected," said Jayram Krishnan, D.O., a urologist at Cleveland Clinic. "They function together to get all the urine out effectively. They usually come out in one piece."
While the most common reason for a cystoprostatectomy is muscle-invasive bladder cancer, other reasons include prostate cancer that is invading the bladder or a bladder where the muscle is nonfunctioning. Radiation therapy or surgery in the pelvis may lead to a defunctionalized bladder.
The current standard for treating men with muscle-invasive bladder cancer is open radical cystoprostatectomy, in which the surgeon makes a large incision in the abdomen, according to Samuel Haywood, M.D., a urologic oncologist at Cleveland Clinic.
During laparoscopic radical cystoprostatectomy, on the other hand, the surgeon removes the bladder and the prostate by making several small incisions. This is less traumatic than an open radical cystoprostatectomy.
"More recently, we've been doing robotic approaches where we dock the robot to the abdomen and are able to use much smaller incisions," Haywood explained. "With that, patients have less blood loss, shorter hospital stay and they're able to go home faster."
What is urinary diversion?
Any time the bladder is removed, the surgeon must find a way for urine to leave the body, which is why cystoprostatectomy is combined with "urinary diversion," Haywood said.
The most common type of urinary diversion is an ileal conduit. To accomplish this, the surgeon disconnects a short portion of the small intestine called the ileum, and then the ureters—tubes that drain urine from the kidney to the bladder—are attached to one end of the ileum, and the other end is attached to a stoma, which is an opening in the abdomen. The ileum acts as a conduit, allowing urine to flow into an external bag called a urostomy pouch. About 70 percent of cystoprostatectomy patients have the ileal conduit done, according to Krishnan.
Another urinary diversion method is the orthotopic neobladder. The surgeon uses a segment of the small intestine to form a new (neo-) reservoir for the urine and then attaches it to the ureters and urethra. The patient is then able to urinate in a manner that is similar to having a bladder.
Potential complications and side effects
The surgery can take six to eight hours, and the patient's hospital stay can last three to seven days. As with any major surgery, complications can arise from a cystoprostatectomy. In fact, more than half of patients have some type of complication after they leave the hospital, according to Haywood. For this reason, he tells patients to count on experiencing a complication or side effect—dehydration, nausea, infection—so they know what to expect and plan accordingly.
The intestinal aspect of the surgery is the most common cause of complications, Krishnan said. When isolating a segment of the intestine to use for the bladder, the surgeon has to then restore the connection for the intestine, and complications are often associated with that part of the surgery.
"It takes time for your intestines to wake up after the surgery," Krishnan said.
Due to the high risk for complications, both Haywood and Krishnan recommend men undergo a cystoprostatectomy at a major medical center staffed with surgeons who handle these procedures regularly. Cleveland Clinic, for example, performs between 150 and 200 cystoprostatectomies each year.
"It's not like other operations because of how intense it is with multiple different things going on," Krishnan said. "There's a risk for bleeding throughout the entire procedure. That would be the biggest thing."
Recovering from surgery
The first question patients usually ask Haywood is, "How is this going to change my life?"
Haywood outlines the life changes they must make, such as caring for their urinary diversion. Many men ask if they will be limited in the activities they can perform.
"We're able to really make them feel better by saying most of the activities they were doing beforehand they're still able to do afterward," Haywood said. "There's obviously a period of convalescence in healing, but for the most part, the urinary diversion should not limit them in their activities going forward."
Krishnan pointed out that the most significant effect for a patient is the psychological impact of not having a bladder and having a bag on their side, should they choose the ileal conduit route.
Following the surgery and hospital stay, patients are typically sent home with pain medicine. Alvimopan (brand name Entereg) is commonly used after the operation because it helps men regain their bowel function sooner.
"Lots of people will give antibiotics for a short course to try to prevent the risk of infection," Haywood said. "The antibiotics have not yet really been proven. We're actually doing a study to try to investigate that."
Haywood mentioned ERAS, or enhanced recovery after surgery, a multimodal, multidisciplinary approach taken by the surgical team that can help patients recover more quickly and ensure they have the best possible outcome from cystoprostatectomy.
How is sexual function impacted?
Sexual dysfunction following a cystoprostatectomy is very common, Haywood said. When the prostate is removed, a man often experiences erectile dysfunction (ED) and won't be able to ejaculate. However, patients can still have an orgasm because it is a brain event and can occur without ejaculation.
A significant number of nerves, for both ejaculation and erections, are associated with the prostate. With nerve-sparing techniques, the surgeon avoids cutting these nerves and helps preserve the erectile function of the penis.
"In order to get an erection, you have the nerve signals and you have to have adequate blood flow," Krishnan said. "Both of those are disrupted when you have this surgery."
According to Krishnan, about 25 percent to 30 percent of cystoprostatectomy cases involve younger men, many of whom choose to undergo nerve-sparing procedures.
The prospect of cystoprostatectomy can be overwhelming, and you need to accept the likely possibility of complications on some level. By putting yourself in the hands of experienced medical professionals, you can ease your concerns and more easily adjust to a new life after surgery.