Study: Using Frozen Embryos in IVF May Increase Hypertension Risk
People who undergo in vitro fertilization (IVF) using frozen embryos may be more likely to experience high blood pressure during pregnancy than those who conceive naturally or use fresh embryos, according to a study published in Hypertension, a journal of the American Heart Association.
“Although most IVF pregnancies are healthy and uncomplicated, this analysis found that the risk of high blood pressure in pregnancy was substantially higher after frozen embryo transfer compared to pregnancies from fresh embryo transfer or natural conception,” lead study author Sindre Petersen, Ph.D., a fellow at the Norwegian University of Science and Technology, said in a statement.
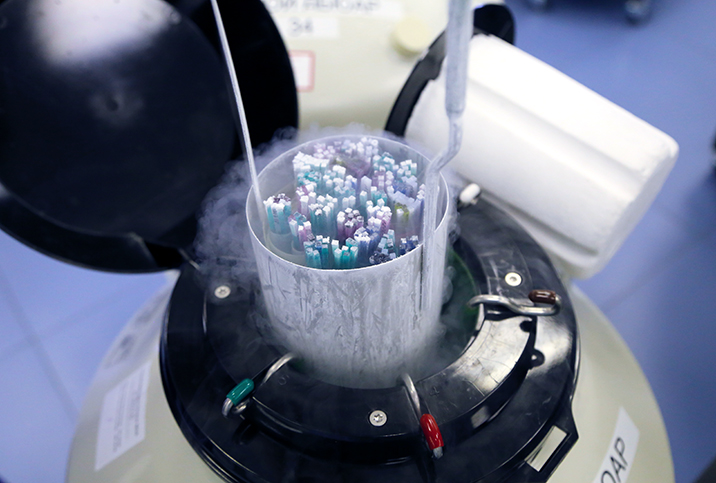
The practice of using frozen vs. fresh embryos has become increasingly common worldwide. That’s largely due to rising interest in fertility preservation—people everywhere are having kids later than their parents. But it’s also because frozen embryo transfers provide certain advantages, explained Lora Shahine, M.D., a reproductive endocrinologist practicing at Pacific Northwest Fertility in Seattle and host of the Baby or Bust podcast.
“In my own career, I have witnessed a dramatic transition from mostly fresh embryo transfers to mostly frozen embryo transfers,” she said, adding that the benefits of frozen embryos include a decreased risk of ectopic pregnancy and ovarian hyperstimulation syndrome, as well as an opportunity for pre-implantation genetic screenings.
In an email interview, Petersen noted that frozen embryo transfer is also associated with a higher likelihood of successful implantation and delivery compared with fresh embryo transfer. Moreover, frozen embryo transfers, especially in an artificial, non-ovulatory cycle, require less planning and are less time-sensitive than fresh embryo transfers.
As a result, in the past few years, some clinics have adopted a “freeze-all” approach, freezing all embryos and foregoing fresh embryo transfers entirely. But according to Petersen, that might not always be the right choice.
About the study
Petersen and his colleagues collated data from the Medical Birth Registries of Denmark, Norway, and Sweden from 1988 to 2015. They looked at about 4.5 million pregnancies, including 4,426,691 that were naturally conceived, 78,300 using fresh embryo transfers, and 18,037 frozen embryo transfers. Participants were 20 to 44 years old. On average, parents who used frozen embryos were 34 years old, while those who used fresh embryos were 33, and those who conceived naturally were 29.
The findings suggest those who used fresh embryos were about as likely as those who conceived naturally to develop hypertensive disorders, the study authors wrote. The use of frozen embryos, however, correlated with a 74 percent higher risk of hypertensive disorders compared to natural conception. Specifically, researchers found the likelihood of developing hypertension during pregnancy was 7.4 percent with frozen embryo transfer and 4.3 percent with natural conception.
Researchers accounted for parental factors such as smoking, BMI, and underlying health conditions. They also performed a “sibling comparison.” Out of all the pregnancies, 33,000 had siblings who had been conceived by different means. The researchers compared the siblings’ pregnancies to determine if the risk was linked to the parent, not the procedure. They found that even among siblings, the risk of hypertension was significantly higher with frozen embryos compared to natural conception.
“Our sibling comparisons indicate that the higher risk is not caused by factors related to the parents, rather, however, that some IVF treatment factors may be involved,” Petersen said in the statement.
Why hypertension is dangerous
High blood pressure can signal preeclampsia, eclampsia and other serious complications that can put the pregnant person and fetus at risk. For this reason, all pregnant people, regardless of conception method, should be closely monitored for signs of hypertension.
“Indeed, hypertensive disorders in pregnancy are one of the leading causes of maternal deaths in the world (especially in the developing world). Furthermore, even in developed countries, if you are diagnosed with a hypertensive disorder in your pregnancy, you are at a higher risk of developing cardiovascular diseases later in life, and the American Heart Association considers a history of preeclampsia as a major risk factor for developing cardiovascular diseases (such as coronary heart disease and stroke),” Petersen wrote.
“Finally, the fetus’ health and growth can be impaired when they are developing in a pregnancy affected by hypertension or preeclampsia, known as intrauterine growth restriction (IUGR) or fetal growth restriction (FGR), as well as a higher risk of preterm birth.”
Why more research is needed
Petersen and his colleagues wrote that their results are consistent with earlier population-level studies suggesting a link between hypertension and frozen embryo transfers. For example, a study presented at the European Society of Human Reproduction and Embryology in 2021 found a higher risk of preeclampsia and hypertension in pregnancies conceived with frozen embryos. However, they say more research is necessary to determine what aspect of the frozen embryo cycle or transfer might contribute to hypertension.
“A theory that is being researched a lot these days revolves around the ‘corpus luteum,’ a temporary endocrine structure which is formed from the remains of the ovarian follicle after ovulation. In programmed frozen cycles (again, also known as artificial cycles and non-ovulatory cycles) the formation of the corpus luteum is bypassed altogether by the clinician, whereas in fresh cycles and natural conception cycles, the corpus luteum secretes vasoactive hormones which could be important for maternal adaptation to the pregnancy,” Petersen wrote in an email.
“This theory remains to be established 100 percent, and other treatment characteristics of the frozen embryo transfer process, for example epigenetic changes associated with the cryopreservation or the thawing process could be involved as well.”
Martha Noel, M.D., a reproductive endocrinologist with Reproductive Medicine Associates in Northern California said there are a number of studies showing the process of IVF, regardless of the embryo transfer method, increases the risk of hypertensive disorders.
“This could be due to infertility itself, the process of culturing the embryos outside the body in the embryology lab, or most likely a combination of the two,” she wrote in an email.
“It’s likely caused by differences in placentation (how the placenta attaches and develops) in IVF versus naturally conceived pregnancies. As you can see from this paper, both fresh and frozen embryo transfers conferred a higher risk of preeclampsia (and a trend towards increased rates of hypertension) as compared to a non-IVF pregnancy.”
“One area of debate is whether or not a frozen embryo transfer in a natural cycle results in lower rates of hypertension and preterm birth than a frozen embryo transfer in a medicated cycle,” she continued. “There are some data that suggest this, but it is still an active area of ongoing research. This study was not able to address this question as it was not able to separate out frozen embryo transfers into natural vs. medicated cycle types.”
What this means for people trying to conceive
Although IVF may increase the risk, some experts say other factors like maternal age or body composition, underlying health conditions, or the presence of multiple gestations are likely to have a much more significant influence. Some of these factors are modifiable, Noel said, with lifestyle and dietary changes or medications. Doctors can also mitigate risks by adjusting their protocol based on a patient’s needs.
Sue Ellen Carpenter, M.D., a fertility specialist at Bloom Fertility in Atlanta, GA, said the study’s results may be statistically significant but are not clinically noticeable. Nonetheless, she said, doctors should provide all pregnant people with comprehensive, individualized preconception counseling before IVF or any other fertility treatment. Petersen agrees.
“Based on our findings, we think that our study emphasizes that careful consideration of all benefits and harms is needed before freezing all embryos as a routine (the ‘freeze all’ approach) rather than for couples with clinical indications, especially given how dangerous preeclampsia can be for both the mother and the fetus,” he said.
“That being said, I am very confident that a well-grounded and individualized decision of whether to go for a fresh or frozen embryo transfer can be made after dialogue between the clinicians and their patients. If our study can contribute by facilitating this informed decision-making, then I am all on board.”