Fifth Person Potentially 'Cured' of HIV

A fifth person may have been cured of HIV, according to a report published earlier this year. Known as the "Dusseldorf patient," the man has lived for four years with undetectable levels of the human immunodeficiency virus (HIV) while off of antiretroviral therapy, nine years after he received a stem-cell transplant.
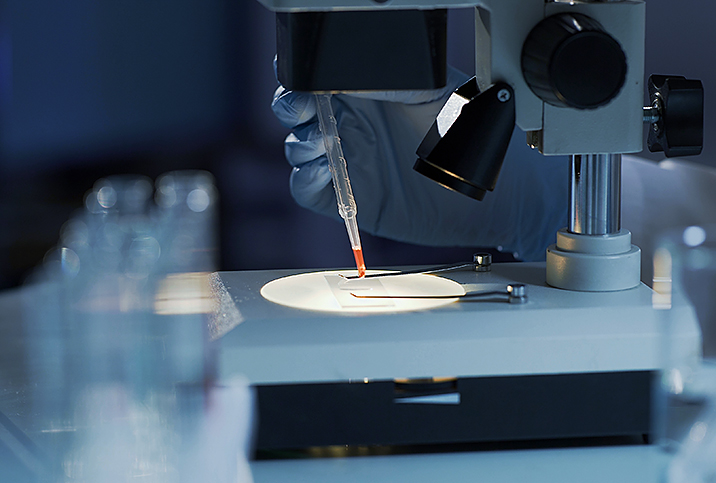
Per the paper published in Nature Medicine, the 53-year-old German, similar to three of the four patients before him, was treated with a transplant of stem cells derived from bone marrow. The technique involves using blood from a donor with a genetic variation that prevents HIV from recurring.
Human immunodeficiency virus is a virus that attacks the body's immune system. If HIV is untreated, its final stage can lead to AIDS (acquired immunodeficiency syndrome). There is currently no approved effective cure.
"Over time, HIV destroys CD4 cells, which are our white [blood] cells important for fighting infections," said Mehri Sadri McKellar, M.D., associate professor of medicine at Duke University and infectious disease physician based in Durham, North Carolina. "HIV infects CD4 cells by attaching to receptors on the cell's surface, including one called the CCR5 receptor. While occurring very rarely (approximately 1 percent of the world's population), a mutation in the CC55 (known as delta 32) can prevent HIV from entering our CD4 cells.
"In stem cell treatment, which is used for leukemia, immune cells are destroyed with chemotherapy," she added. "Then new cells are given back to the patient using donor cells."
Other than leukemia, hematopoietic stem cell transplantation (HSCT) is used to treat lymphatic system cancers. Stem cell therapy can be used to treat a range of conditions, such as autoimmune, inflammatory and neurological disorders, and burns and traumatic injuries.
When cancer isn't present, chemotherapy and radiation aren't necessary. Because these therapies carry a high risk of side effects and complications, experts said using them for people living with HIV, who don't have cancer would be unethical.
However, for the few people with both conditions, the treatment can deliver a one-two punch to eradicate HIV and cancer simultaneously.
"Even without anti-retroviral medication, the HIV in a patient's body can no longer infect the new HIV-resistant blood/immune system and no longer replicate in the body, resulting in HIV remission or potential cure," said Jingmei Hsu, M.D., a hematologist in New York City, who used the same method to treat another patient, known as the "New York patient" at New York-Presbyterian/Weill Cornell Medical Center.
Antiretroviral medication (or ART therapy) can reduce HIV to nearly undetectable levels (U=U, undetectable = untransmittable), which means it cannot be transmitted to another person or develop into AIDS, according to the Centers for Disease Control and Prevention (CDC).
With ART, people with HIV can live long, healthy lives, but the virus remains in the body and can resurge if they stop taking the medication. Experts consider a person "cured" of HIV if they have discontinued ART and continue to have undetectable levels of HIV years later.
The Dusseldorf patient stopped taking ART in 2018.
Who else has been 'cured' in this way?
The first person to be treated and successfully cured of HIV using a stem cell transplant was Timothy Ray Brown. Brown, referred to as the "Berlin patient," discontinued HIV treatment on the day of his transplant and lived for 12 years with undetectable virus levels before dying of cancer in 2020.
The second person, Adam Castillejo, known as the "London patient," was in remission for 30 months as of 2022 after receiving a blood transplant for Hodgkin's lymphoma, which affects the lymphatic system, per the American Foundation for AIDS Research (AmfAR).
A third man, a 66-year-old, was treated in Duarte, California. He has been in remission for HIV since 2019 after receiving stem cell therapy to treat acute myelogenous leukemia, an aggressive cancer of the blood and bone marrow, according to an announcement in the American Journal of Managed Care.
The fourth person, known as the "New York patient," was declared HIV-free in 2022, according to the World Health Organization (WHO). Unlike the others, her donation came from an umbilical cord.
Why the 'New York patient' is unique
The New York patient was the first woman and person of mixed race to be potentially cured of HIV, according to the case report. Upon being diagnosed with the virus in 2013, she was diagnosed with acute myeloid leukemia in 2017, and received a blood transplant the same year.
In 2023, about 30 months after stopping HIV treatments, she had yet to experience any signs of either HIV or leukemia returning, per the National Institutes of Health (NIH).
After receiving the umbilical cord blood, the woman received another blood donation from a close relative. Although umbilical cord cells are more adaptable, cord donations don't yield sufficient supply for adult recipients. The adult cells correct the deficit and support the growth of the new immune system to increase the likelihood of safe and successful transfer.
Experts said that despite the need for an additional adult donation, cord blood was a crucial factor.
"What is different about this treatment is that they used stem cells from umbilical cord blood versus from bone marrow," McKellar said. "It is easier and less invasive to obtain stem cells this way. Also, since stem cells in cord blood are more 'immunologically naïve'—that is, they haven't been exposed to infection—there is less chance of a rejection and/or a mismatch between the donor and recipient."
In addition to being more "adaptable" and widely available, experts said cord blood doesn't need to be precisely matched to the recipient. Typically, a match must be nearly exact to prevent the immune system from rejecting the new blood.
For people of color (BIPOC) and those of mixed ethnicities, finding such a match can be challenging because most donations in blood banks come from donors of Northern European heritage.
Experts said it is even more difficult to find a match that also possesses the genetic variation necessary to protect against HIV, especially for BIPOC people, because that variation exists primarily in people of Northern European descent. Of all people living with HIV in the United States, 28.5 percent are white, 40.3 percent are Black and 24.7 percent are Hispanic, according to CDC statistics.
The ability to use a partially matched graft from an umbilical cord could potentially benefit dozens of the 1.2 million people living with HIV in the U.S., experts said.
Hsu said about 48 percent of HIV infections worldwide occur in female-identifying people. The report of the first potentially cured female-identifying person should provide hope to others living with the virus.
"I think this has huge symbolic implications that women can also benefit from such a treatment approach," Hsu explained. "It is also important to point out that people with non-white backgrounds will also be able to benefit from such an approach."
Other available HIV treatments
Stem cell therapy is currently only viable for people living with HIV who have certain types of aggressive cancer, and all treatments have not been successful.
"This is a great step in understanding what it takes to cure HIV," McKellar said. "However, this treatment is not ready for prime time. It is expensive, invasive, risky and has only been studied in persons with leukemia."
Nonetheless, experts emphasized cases such as the Dusseldorf patient are crucial.
"Before these types of cases, we did not know that a cure was possible," said Luis J. Montaner, D.V.M., D.Phil., a disease expert at the Wistar Institute in Philadelphia who studies the mechanisms of conditions such as HIV, cancer, COVID-19 and emerging viral infections.
These success stories indicate it is possible to eradicate HIV from the body, he said, and have set a foundation for future research.
Moreover, stem cell therapy is just one of many developments in HIV prevention and management to arise in the past 40 years, McKeller added.
"There is a lot of work being done on developing an HIV cure as well as an HIV vaccine, especially as technology improves," she continued. "In terms of HIV treatment, we are now using injectable medication that can be administered every two months which has been a game changer for persons who struggle with daily pills. More injectable medications are on the horizon, including some which are every six months."
About 75 percent of the 38 million people living with HIV in the world receive ART, according to UNAIDS (The Joint United Nations Programme on HIV and AIDS).
Additionally, many people use preexposure prophylaxis (PrEP), an antiviral treatment that can diminish the risk of contracting HIV. PrEP is 99 percent effective at preventing HIV transmission through sex and 74 percent effective at preventing it in people who inject drugs, according to the CDC.
"The majority of my patients have undetectable HIV viral loads—which means they have no active virus in their system putting them at risk for infection, nor can they transmit to others," McKellar said. "It's been an amazing success."