The Evolving Accepted Wisdom Surrounding the Prostate
Certain misconceptions have constantly surrounded the prostate. It's a mysterious gland most men couldn't point to on a map of their anatomy, which makes it easy to hear and accept information as fact without scientific scrutiny. That's an issue.
Another problem for the layperson is that even medical knowledge and wisdom regarding the prostate is changing as science discovers more.
Let's look at a few of the traditional nuggets of insight that have never been true before diving into the accepted wisdom, which has changed over time.
Sanjay Pandey, M.S. (master of surgery), a urologist and the head of andrology and reconstructive urology at the Kokilaben Dhirubhai Ambani Hospital and Medical Research Institute in Mumbai, India, highlighted three of the most common misbeliefs:
- Prostate issues occur only in older men. Not true. Young men can also face prostate cancer and other conditions.
- The larger the prostate, the more the potential symptoms. Another myth. A small prostate can also be occlusive and cause urinary problems, too.
- Prostate cancer is always a dangerous disease. Again, not necessarily the case. Some prostate cancers can be very slow-growing and never threaten someone's life.
These historical beliefs have been challenged, and knowledge about the prostate has progressed significantly in recent times. It's a good bet some other tidbits have changed of late, as well, beginning with the most prominent prostate cancer test.
The PSA's shifting reliability
The prostate-specific antigen (PSA) test has traditionally been one of the main tools physicians use when screening for prostate cancer. But it isn't perfect, and elevated PSA levels don't always point to prostate cancer; rather, they could be the result of other conditions or medications.
"For decades, over-testing PSA without looking into additional clinical parameters has led to unnecessary invasive biopsies," Pandey said. "Gene-mapping tests have now overtaken the identification and prediction of prostate cancer."
The PSA test is still in use, but its prominence and clinicians' reliance on it are changing. This is no surprise given it has always been a weak specific screening test for prostate cancer, according to S. Adam Ramin, M.D., a urologist and the medical director of Urology Cancer Specialists in Los Angeles.
"Many men with elevated PSA do not have prostate cancer," Ramin said. "In the past, patients with elevated PSAs would need to undergo a prostate biopsy to determine the presence of prostate cancer."
However, relying on a PSA test alone has led to unnecessary treatment in some cases. About 3 in 4 men with an elevated PSA level will not have cancer, according to the United Kingdom's National Health Service (NHS), because the PSA test cannot distinguish between slow-growing, harmless cancers and aggressive, potentially lethal cancers, stated the National Cancer Institute.
"Now, with recent advances in other testing, men with elevated PSAs may be eligible to initially undergo additional tests to determine the likelihood of the presence of significant prostate cancer," Ramin said. "Once a man has completed these other tests, a prostate biopsy may be recommended."
As Ramin noted, testing for prostate cancer has progressed, no longer relying on the PSA test alone. Four of the newer approaches include:
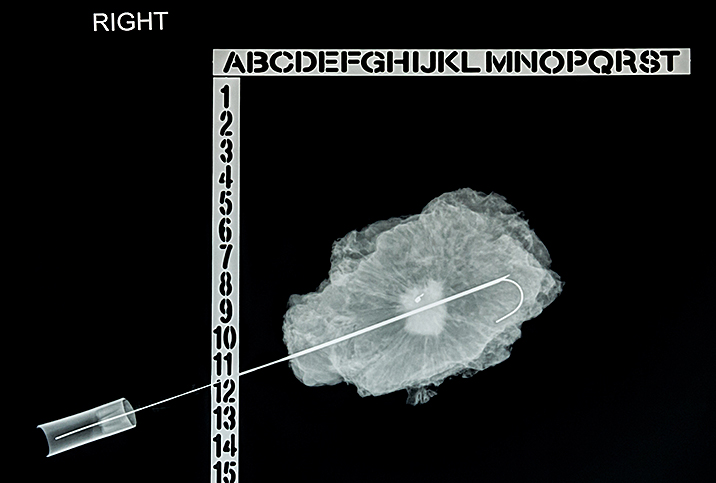
- MRI of the prostate. Magnetic resonance imaging (MRI) uses a magnetic field, radiofrequency pulses and a computer to produce a detailed picture of the prostate.
- PSA 4K score. This is a blood test that measures the levels of four substances from the kallikrein family of enzymes, in conjunction with other clinical information such as age, rectal examination findings and the results of any previous biopsy. The final result is a percentage score showing a patient's risk for aggressive prostate cancer.
- Urinary molecular testing. The PCA3 test can detect PCA3 and the TMPRSS2-ERG gene fusion, which are prostate cancer biomarkers. Using these two biomarkers in combination can help reduce unnecessary biopsies, according to the National Cancer Institute.
- Liquid biopsies. This advancing area of cancer detection and treatment can identify cancer cells in the blood.
These additional tests can help doctors determine whether men with a slightly elevated PSA level should undergo a prostate biopsy. Clinicians can also use these tests to determine if a man who previously had a negative prostate biopsy but is experiencing a continuously rising PSA should have a second biopsy.
Prostate treatment options have vastly improved
According to Ramin, there have been advancements and changes in the treatment of prostate cancer for men with localized disease and metastatic disease. A biopsy isn't the default choice anymore.
"For localized prostate cancer, minimally invasive treatments such as high-intensity frequency ultrasound [HIFU], cryotherapy and robotic surgery have revolutionized treatment options for men with prostate cancer," he said.
Many patients with less aggressive localized prostate cancer may not even need treatment, but rather active surveillance.
"We can better determine which patients with prostate cancer can be placed on an observation protocol called active surveillance rather than undergo treatment," Ramin said.
The state of genetic molecular testing in the past 10 years has significantly advanced, according to Ramin. This testing aids urologists and patients in determining the possibility of tumor progression versus a tumor remaining dormant.
"Patients with less aggressive, more dormant-type cancers are good candidates for active surveillance," he said.
In addition, Ramin and Pandey both indicated there have been advances in the treatment of patients with large prostates, which is attributable to a shift to newer modalities of minimally invasive therapy, Pandey said.
"Over the past 10 years, surgical techniques have developed so that men with markedly large benign prostatic hyperplasia [BPH] can now undergo minimally invasive robotic surgery," Ramin said, adding that even less-invasive treatment options with reduced complications have also been developed for BPH, such as prostatic urethral log (UroLift), intraprostatic steam injection (Rezūm) and water therapy (Aquablation).
With the evolving knowledge of the prostate and the availability of more accurate tests, how have prostate screening guidelines changed?
Recommendations about when to start prostate exams
Beyond testing and treatment, current wisdom surrounding prostate exams and screening has undergone a shift due to a change in recommendations on prostate cancer made by the U.S. Preventive Services Task Force, Ramin said.
In 2012, the task force released guidelines suggesting the harms of PSA testing for men outweighed the benefits. Ramin explained that this body of scientists, government officials and physicians made recommendations that dissuaded primary care physicians from broad-ranged PSA testing and rectal exams.
"On the face of it, these recommendations were well-meaning, namely, to reduce the overtreatment of prostate cancer," Ramin said, adding there have been some unintended consequences. "As primary care physicians decreased their screening for prostate cancer, we noted a spike in cases of more aggressive and more advanced prostate cancers. In other words, the delay in screening for prostate cancer may have inadvertently led to prostate cancer being discovered at the later stages."
In 2017, the task force changed these recommendations, stating adults between the ages of 55 and 69 should discuss the pros and cons of PSA tests with their doctor before deciding about screening. The task force also stated men older than age 70 should not have routine PSA tests for prostate cancer.
Guidelines for prostate screening differ slightly from country to country. For example, in the United Kingdom, you have the right to a PSA test if you're older than 50 and you've thought carefully about the advantages and disadvantages.
Looking after your prostate health
This brings us to some important recommendations regarding prostate health.
"We urge all men over age 50 to ask their primary care physicians for prostate cancer screening," Ramin said. "The PSA test, while not accurate, is still the best initial test, alongside a rectal exam, for cancer screening."
Pandey agreed with this point, saying it is best for men in their 50s to get their prostate evaluated by a physician who is using a combination of thorough clinical examination and PSA testing.
"While we do not advocate performing prostate biopsies on every patient with elevated PSA, the initial step to perform screening is still essential," Ramin advised.
Furthermore, Ramin stressed that men with a family history of cancer—a father or brother with prostate cancer or a mother or sister with breast cancer—should consider getting a PSA test and a rectal exam at the age of 40.
"Lastly, it is also important to note that one PSA test is not enough," Ramin said. "It is recommended that men undergo PSA testing either yearly or every two years. While these are broad-based recommendations, a patient's healthcare provider can give more personalized recommendations specific to their circumstances."