If You Suffer Eczema, Watch Out for Stress-Induced Flare-Ups

The skin is the largest organ of the body with a total area of about 20 square feet—though it's often the most neglected part of your body, which can be concerning, since your skin often manifests other issues happening within your body. People with eczema know this better than most and should take special care.
About those sebaceous glands…
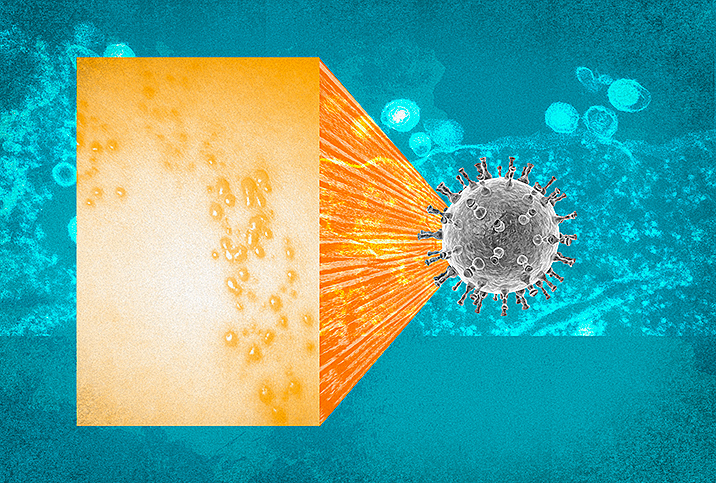
Although there are several types of eczema, studies show seborrheic dermatitis is the type most often triggered by stress.
"Seborrheic dermatitis/eczema is an inflammatory skin condition caused by an overgrowth of yeast which reacts negatively with the oils on the skin," explained Tristi Edwards, a Jamaica-based dermatologist. "It's common and noncontagious. 'Seborrheic' refers to the sebaceous glands, while 'derm' means skin. It's called dandruff—or pityriasis capitis—when it's found on a teenager's or adult's scalp, and 'cradle cap' when it's on a baby's head.
"Seborrheic eczema manifests as occasionally itchy, red, lighter or darker greasy flaking to the scalp, central face, ears, chest and back most commonly (areas of skin with more sebaceous glands)," she added. "Persons often note a flare of this condition when going through a stressful period, e.g., a major exam."
Who's at risk?
An estimated 11 percent of the population has seborrheic eczema, affecting mostly infants younger than 3 months old and adults between the ages of 30 to 60 years. Men are more prone to outbreaks than women, and caucasians tend to have higher incidences of seborrheic eczema than Black Americans.
A family history of psoriasis can increase your odds of developing seborrheic eczema, as well as having naturally oily skin.
Certain health issues create a risk of developing seborrheic eczema, such as immunosuppressions caused by organ transplant, adult Hodgkin's and non-Hodgkin's lymphoma, and HIV. Also, certain psychiatric disorders, neurologic diseases and congenital disorders can increase risk: depression, Parkinson's disease, epilepsy, tardive dyskinesia, facial nerve palsy, spinal cord injury and Down syndrome.
Taking psychotropic medications like lithium, buspirone, haloperidol decanoate and chlorpromazine has also been linked to seborrheic eczema.
Identifying when stress triggers your eczema
Kathey, a college lecturer in Kingston, Jamaica, has had eczema since childhood, experiencing painful itchy sensations on the back of her thighs as early as 7 years old. One particular spike of the disease "coincided with a horrible acne breakout, which was triggered by my parents' announcement that they were getting a divorce," she said. "During my diagnosis of stress-related adult acne, my dermatologist discovered that my acne was triggered by my eczema and that while treating eczema it further exacerbated the acne."
Controlling the condition through her 30s proved difficult, with breakouts affecting the back of her knees, thighs or the crease on the inside of her elbows. In some areas it looked like a regular rash; in others, like on her thighs, it looked like ringworm.
During a particularly stressful period at work during 2019, she had her worst outbreak.
"At first, there were just some watery, chicken-pox-looking bumps on the outside of my palm and along the inside of my fingers," she explained. "Then, as the bumps multiplied, they merged together to form very painful pus-filled blisters. They took over my entire hands. Some got infected, and this made it very painful to stretch my fingers out. It was so painful that I literally could not take care of my then 3-year-old daughter. It was very embarrassing to go out in public because my hands looked like that of a leper—and itched like it."
Controlling and treating stress-induced eczema
Stress isn't just a psychological condition as it has far-reaching effects on the organ systems, including your skin. Stress can affect immunity and lead to general inflammation in the body. At the level of the skin, stress hormones can induce increased production of sebum from the sebaceous glands in the hair follicle. This excess sebum production, coupled with the overgrowth of yeasts and background inflammation, triggers flare-ups of seborrheic dermatitis.
"Seborrheic eczema, unfortunately, cannot be cured," Edwards advised. "However, you can gain control over the condition and minimize flares. And first and foremost, finding different ways to minimize stress is recommended. When unusually widespread, further investigations are necessary to rule out immune system suppression due to underlying causes. Products such as antifungal creams and shampoos, anti-inflammatory creams/ointments, sulfur and salicylic acid are some of the treatments we have in our armamentarium to tackle seborrheic dermatitis and keep it under control."
In mild cases, over-the-counter dandruff shampoos that contain selenium, zinc pyrithione or coal tar can help. Long-term care often requires a prescription from a healthcare provider for antifungal shampoos that contain ciclopirox (Loprox) or ketoconazole (Nizoral). Moderate to severe cases may require a shampoo containing betamethasone valerate (Luxiq), clobetasol (Clobex), fluocinolone (Capex) or fluocinolone solution (Synalar).
'You can gain control over the condition and minimize flares. And first and foremost, finding different ways to minimize stress is recommended.'
You can treat flare-ups on the face and body with topical antifungals, corticosteroids and calcineurin inhibitors. Creams, foams and gels with the main ingredients ciclopirox, ketoconazole or sertaconazole can also be helpful.
Topical corticosteroids that include betamethasone valerate, desonide, fluocinolone or hydrocortisone are usually available in creams, lotions, foams, gels, ointments, oil or solution. These are often prescribed if antifungals are not effective. Corticosteroids can cause a thinning of your skin and should not be used continuously for weeks or months at a time without a break. Pimecrolimus cream (Elidel) or tacrolimus ointment (Protopic) are calcineurin inhibitors, and are prescribed as alternatives to corticosteroids.
While seborrheic eczema is uncomfortable, and at times painful, it is fairly common and completely manageable with the right healthcare advice, treatment your doctor recommends and whatever you can do to manage your stress levels.