What to Expect From a Dilation and Curettage

If you have endometriosis, heavy periods or menstrual complications, your doctor may have mentioned performing a dilation and curettage to diagnose and manage your symptoms. This minor surgical procedure allows your gynecologist to perform diagnostic testing that will better inform your treatment plan. Like any procedure, a dilation and curettage comes with risks, and understanding the process can help you make an informed decision with your gynecologist.
What is a dilation and curettage?
A dilation and curettage (D&C) is a two-part procedure in which your gynecologist dilates your cervix to access the inside of your uterus. To begin the dilation, your doctor will give you a combination of medications to relax your cervix and gradually insert metal rods to open your cervix.
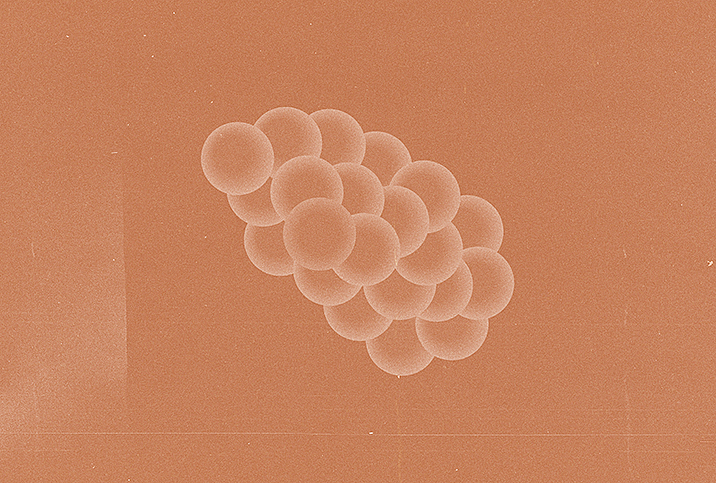
Your doctor will then use a scoop (a curettage) or suction device to remove the lining of your uterus. The goal of this procedure is to remove uterine growths and to reduce the thickness of your uterine lining to help treat heavy periods or remove remnants of the uterine lining following a miscarriage or abortion. Your doctor will take a sample of this lining and send it to a laboratory for testing. This is a routine process that your doctor follows to rule out any reproductive cancers or complications.
A D&C is a simple and common procedure that only takes about 20 minutes to perform. Depending on your symptoms, your doctor may also perform a hysteroscopy, which involves inserting a camera into the uterus to find uterine fibroids, cysts or any indication of chronic reproductive complications that could impact your cycle or fertility.
The risks of a D&C
A dilation and curettage is often performed under anesthesia and is typically an outpatient procedure. You will likely return home the same day as the surgery. Like any procedure requiring anesthesia, your medical history can influence how your body responds to the anesthesia. You may feel dizzy, disoriented and extremely tired after the procedure.
The D&C removes the lining of your uterus that you would normally shed during menstruation, so it's common to have light bleeding immediately following the procedure and for a few days thereafter. You will likely experience cramping and bloating just as you would during your usual menstrual period.
Your cervix will remain dilated after the procedure, and it will take a few days for it to return to its natural size. During this time, your uterus is more susceptible to infection, so you should avoid using tampons or menstrual cups following the procedure, and avoid having sex as this is the easiest way to introduce bacteria into your vagina that could cause a cervical or uterine infection.
It's also important to closely monitor your bleeding following the surgery because it should be minimal. If you pass clots or experience heavy bleeding, you should contact your doctor immediately as this may be a sign of a perforation.
After the procedure
Although this is a simple surgery, you are at a higher risk for infection, so it's important to take your time and allow your body to recover.
Your gynecologist will schedule a follow-up appointment to discuss your recovery and the results of the laboratory screenings. This follow-up is essential for your reproductive health as your doctor can explain the findings and your treatment plan. This appointment can also identify possible adhesions (or scar tissue), which can develop after any surgical procedure and impact your fertility.
The biggest challenge following a D&C can come from family and friends who do not understand your condition and need for the procedure. For many women, a dilation and curettage is the first step in helping improve fertility and to diagnose chronic conditions, but a D&C is most commonly understood as the medical term for an abortion. Unfortunately, this misconception keeps many women from discussing how useful a D&C is in diagnosing endometriosis and treating uterine fibroids. Understanding this use of the procedure can help normalize its usage in maintaining women's reproductive health.