After Screening: How to Diagnose and Treat Colorectal Cancer
Colorectal cancer is the name given to any cancer that develops in the colon (the bulk of the large intestine) or in the rectum (the final section of the large intestine). An estimated 151,000 new cases of colorectal cancer were diagnosed in 2022, representing 7.9 percent of all new cancer cases, according to SEER data from the National Cancer Institute.
Colorectal cancer is the fourth-most common type of cancer but the second-deadliest, killing an estimated 52,000 Americans in 2022 alone.
The five-year relative survival rate for colorectal cancer is 65.1 percent, meaning two-thirds of people diagnosed with it live at least another five years. As with any cancer, early detection can dramatically improve those odds, with the five-year relative survival rate jumping to 91 percent when colorectal cancer is detected in the local stage.
Regular colonoscopy screenings at the appropriate age, with consideration for your risk factors, are important.
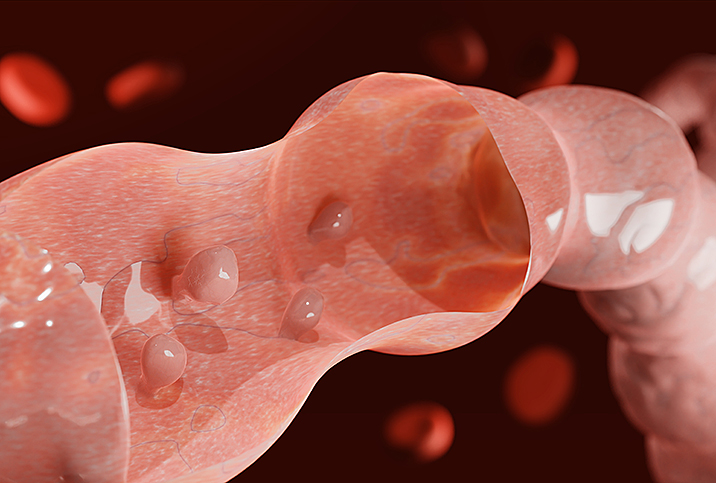
A colonoscopy is a procedure that millions of people around the world undergo every year in order to find and remove any colon polyps before they can develop into cancer. In addition to screening, the humble colonoscopy also plays a significant role in diagnosing colorectal cancer.
It's important to learn what goes into diagnosing colorectal cancer, what some of the treatment options are and what you can do to prevent it—or at least reduce your chances of developing it—in the first place.
Diagnosing colorectal cancer
Despite the existence of other colorectal cancer screening methods, such as a virtual colonoscopy and stool tests that look for hidden blood in your feces, colonoscopy remains the gold standard for screening. It's also a first-line modality for diagnosis.
The diagnostic colonoscopy is more or less identical to a screening colonoscopy, only with the goal of identifying and biopsying any suspect polyps or lesions. Just as with a screening colonoscopy, the patient is sedated, and the doctor passes a long, thin tube into the rectum that contains smaller tubes with a camera, a light and snipping tools. There, it travels all the way to the end of the large intestine or colon.
As the doctor draws the scope back out, they carefully examine the walls of the colon, looking for suspicious growths from which they snip off tissue samples. These biopsied samples are then collected and examined in a lab to see if they're cancerous.
"There are a few benign polyps that don't have cancer potential, and those don't require removal," explained Shahrad Hakimian, M.D., a gastroenterologist with UCLA Health in Los Angeles. "But the vast majority of polyps we find, which we call adenomas, are precancerous and require endoscopic removal. And all of those are sent to a pathologist after their removal, and they look at it under the microscope to determine what it is and make sure there are no more advanced or concerning changes."
If rectal cancer is suspected, the doctor will likely do an exam using another instrument called a proctoscope. It's a thin, rigid, lighted device that allows close examination of the walls of the rectum to identify, assess and measure any tumors that might be present.
Further diagnostics
If your doctor suspects colon cancer, they may order a blood test that looks for a certain chemical biomarker that colon cancer produces called carcinoembryonic antigen (CEA). This test alone can't determine if and to what extent you have cancer, but it can help your doctor track and better analyze your prognosis.
At this point, if you've been diagnosed with cancer, the next step is to determine the extent or stage of the cancer. These stages are indicated by Roman numerals from 0 to IV. The lowest number indicates cancer that's localized to the lining of the colon. The highest means cancer has spread—metastasized—to other parts of the body.
The pathologist analyzes the biopsied tissue, and you may be referred for other tests to further define the parameters of the cancer if it's confirmed.
"We'll take biopsies of that lesion and send it to a pathologist who basically does a confirmatory tissue diagnosis," Hakimian said. "And once they do that, depending on the size of the lesion and the location and other characteristics, we may recommend additional imaging tests to basically determine if now this cancer we've detected is localized in that area or if there's evidence of spread elsewhere, usually a CT scan. But a regular CT alone is not a good enough test to definitively diagnose cancer. It's usually for once we have a tissue diagnosis; it helps us determine more the spread of that cancer or lesion."
Treating colorectal cancer
Every cancer is different and requires unique analysis and treatment. However, there are certain general approaches that are typical for various stages of colon cancer.
"Stage 0 is a very superficial cancer that may be occasionally endoscopically resectable and may not need surgery," Hakimian said. "If there's no distant spread, patients usually meet with both an oncologist and a surgeon. And if they're the right candidate, surgery is usually the next thing to consider to better evaluate the cancer, potentially remove it and also better stage the lesion."
With stage I cancer that's localized to a polyp with no cancer around the edges of it, you might get away with just having that polyp removed. However, if it's high-grade cancer or there's cancer at the edges of the polyp, you might need more surgery.
Stage II and stage III cancers almost always lead to partial colectomy, the removal of a section of the colon. Stage IV means the cancer has spread to distant organs, and surgery may not be helpful at that point.
Surgery for colorectal cancer takes place in a sensitive area of the body.
"Typically, for cancer surgery, you don't need to remove the entire colon, you only remove a third or half of the colon," Hakimian said. "In the case of a stage I, occasionally surgery alone can be curative. But if the patient has stage II or stage III, they may need more than surgery. They may need chemotherapy as well to treat the lesion better. A lot of that is patient-dependent. It depends on their health status and their goals and becomes a discussion with an oncologist."
Rectal cancer is a whole different animal. The muscles in your rectum help control your bowel movements, and if there's a need to remove a significant amount of muscle tissue, incontinence is a concern.
In those cases, an ostomy—a surgically created opening in the abdomen that allows waste to be collected in a pouch outside the body—may be needed.
Keep in mind, too, that surgery for colorectal cancer takes place in a sensitive area of the body. One of its side effects for men is potential erectile dysfunction (ED). It's not guaranteed to happen, but it is a possibility. Discuss it with your doctor.
Preventing colorectal cancer
Screening is a vital method of preventing colorectal cancer.
Gastroenterologists may tell you truthfully that many people survive colon cancer treatment and live happy, fulfilling lives. Treatment has come a long way, without a doubt. At the end of the day, however, they may also tell you that you really, really want to avoid all that, if possible.
By some estimates, 75 percent to 90 percent of colon cancer is preventable if only people would just get screened at the appropriate age for their risk factors, including family and genetic history.
You can find a closer look at the lifestyle-based risk factors for colorectal cancer here, but the basics of lowering your risk for the disease include the following:
- Eat a high-fiber diet with lots of fruits and vegetables.
- Avoid too much meat cooked at high temperatures and heavily processed food.
- Stay active.
- Keep your weight under control.
- Avoid tobacco and heavy alcohol use.
Be aware that the latest screening recommendation is age 45, and that's for people at average risk. If you're at higher risk, your doctor might recommend screening at an even younger age.
No matter your age, it's never a bad idea to at least talk to your doctor about screening.
"We've started to detect more colon cancers at an earlier age," Hakimian said. "That has increased over recent years. We don't fully understand why it's happening. Maybe it has something to do with the environment or what we're eating or maybe it's some genetic factor. But that has changed over time."
Don't overlook the power in your own hands to keep yourself healthy, especially for prevention of colorectal cancer. Understanding your risks, your family history and when you should start thinking about screening is a significant first step to avoiding the worst.
Talk to your physician about colorectal cancer screening. Don't have a doctor you see regularly? You should find one. In a bit of good news, telehealth makes it easy to connect with a doctor who can take your personal and family health history and evaluate your situation. Many physicians offer video visits and have same-day appointments. Giddy Telehealth is an easy-to-use online portal that provides access to hundreds of healthcare professionals whose expertise covers the full scope of medical care.