Some at Low Risk for Colon Cancer May Need Fewer Colonoscopies

A colonoscopy is the most effective way to detect—and perhaps prevent—colorectal cancer.
Unfortunately, the potentially lifesaving exam is viewed with an air of dread by too many people. One study found that of 997 middle-aged subjects at average risk of developing colorectal cancer who were making a routine visit to their primary care physician, only 38 percent of those advised to get a colonoscopy underwent any type of colorectal cancer screening during the ensuing year.
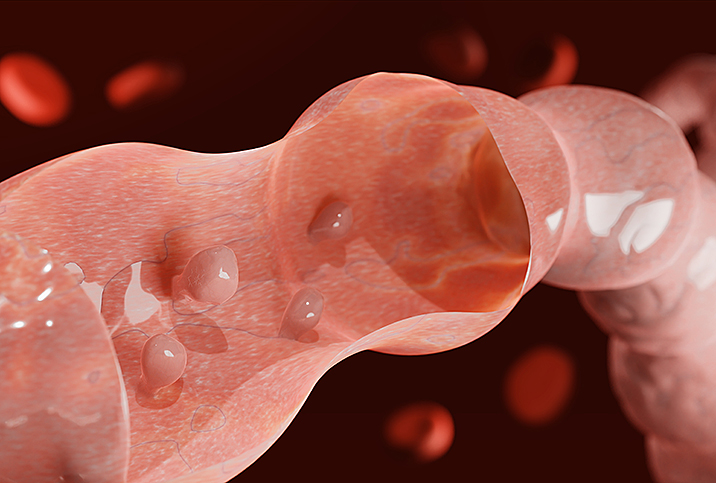
The primary reasons most people avoid colonoscopies? They think the test will be invasive, uncomfortable and inconvenient. You could consider the procedure invasive. A gastroenterologist inserts a colonoscope—a long tube with a light, a camera and a tool to cut polyps—into your rectum and up into your colon, but you are asleep after receiving an anesthetic.
The discomfort and inconvenience come the day before the procedure when you have to drink a strong laxative to clean out your intestines and bowels. You can't eat and can consume only clear liquids. It's unpleasant, but not an excuse to skip the screening.
What is colorectal cancer?
The benefits of colonoscopies far outweigh their unpleasantness, though, according to Haleh Pazwash, M.D., a gastroenterologist at Gastroenterology Associates of New Jersey, which has multiple locations.
"Colonoscopies can really make a difference in someone's life span," Pazwash said. "If we find colorectal cancers early, they can not only be treatable, but they can also be curable."
Colorectal cancer—sometimes also referred to as colon, rectal or bowel cancer—is the third-leading cause of cancer-related deaths in the United States in both men and women, and the second-most common cause of cancer deaths when numbers for men and women are combined.
The current recommendation for a healthy person at average risk is to begin colonoscopy screenings at age 45. If the screening finds no polyps, the person can get a follow-up every 10 years through age 75.
But new research from Germany, published in JAMA Internal Medicine, suggests certain people may be able to safely extend that window and undergo the screening procedure less frequently.
About the study
The German researchers pulled data for the years 2013 through 2019 from a German colonoscopy registry. They examined 120,298 colonoscopy screening patients ages 65 and older who had a previous negative screening at least 10 years before.
They compared their results to all colonoscopies performed on people 65 or older in that time period, which included 1.25 million people.
The researchers discovered that the existence of precancerous or cancerous growths was 40 percent to 50 percent lower among repeat colonoscopy patients. The prevalence of advanced abnormal growths was 3.6 percent in women and 5.2 percent in men 10 years after a negative screening colonoscopy.
The team found those rates rose to 4.9 percent in women and 6.6 percent in men among patients who had a negative colonoscopy 14 years ago or longer. That is compared to 7.1 percent and 11.6 percent, respectively, among all screening colonoscopies during the same time period.
The study authors noted that advanced growth prevalence was at least 40 percent lower among females than among males 10 years or more after a previous negative screening. The presence of abnormal growths was particularly low in women younger than 75, even at windows of up to 13 years.
What the results suggest
The findings suggest that the risk of finding cancerous or precancerous growths a decade after a negative colonoscopy is low. It may be possible to safely extend the 10-year window between colonoscopies, "especially for females and younger participants without gastrointestinal symptoms," according to the study authors.
"Women at younger screening ages with no finding at an index colonoscopy could possibly be screened at prolonged intervals or, alternatively, be offered less invasive methods, such as stool tests, while maintaining the 10-year interval for men and women at older ages," the authors wrote. "By reducing the burden of testing in those at lower risk, such risk-adapted intervals could promote a more efficient use of colonoscopy capacities and resources."
How often should you get a colonoscopy?
Whether you should adhere to the universally recommended 10-year gap between screenings depends on your personal risk level, according to Pazwash, who was not involved in the study.
"A normal-risk person is someone who is healthy, has no family history and no symptoms, meaning they don't have bleeding, abdominal pain or weight loss," she said.
High-risk people, on the other hand, are patients with inflammatory bowel disease, such as Crohn's disease and ulcerative colitis, or patients with a prior history of polyps, she explained.
Polyps are small clumps of cells that form on the lining of the colon. Most polyps are harmless but can develop into colorectal cancer over time.
A family history of colorectal cancer is a major risk factor, Pazwash said.
"If you have a family history of colon cancer, you should not wait 10 years," she stressed. "If you have a family history of Lynch [syndrome], which is superaggressive colon cancer that affects multiple generations, you may need to get colonoscopies yearly."
Between colonoscopies, there are other, less invasive ways to test for colon cancer.
"One option is the Cologuard test, a noninvasive test that looks at different biomarkers in the stool. It is covered by insurance for [people] 45 [and] over," Pazwash said.
Another option is a fecal immunochemical test (FIT), which checks your stool for blood, she noted.
Anyone who is 45 or older should talk to their doctor about what type of test and frequency they recommend based on individual health circumstances and history.
If you are approaching age 45, or have passed it already, and don't have a regular physician, you really need to find one. It's easier than it used to be, given the prevalence of telehealth. Video visits are a regular part of many physicians' practices, and they're a good way to see a doctor quickly, as many offer same-day appointments. Then, if follow-up is required—perhaps a colonoscopy—you have your foot in the door. Giddy telehealth is an easy-to-use online portal that provides access to hundreds of healthcare professionals whose expertise covers the full scope of medical care.
In the end, no matter what your situation or background, the important thing is to get tested.