Delayed Sleep Phase Syndrome May Be Why You're a Night Owl
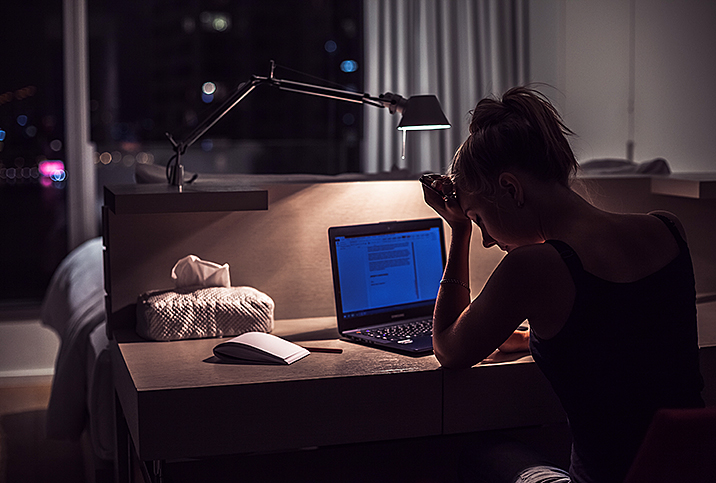
It's 4 a.m. and I'm lying awake in bed—again. I'm scrolling through my phone and probably won't fall asleep for another half-hour. It's not because I want to stay awake at this ungodly hour nor do I enjoy tossing and turning for what feels like forever while I'm chasing zzz's.
I've regularly gone to bed and fallen asleep at this hour for years. But why?
Ever since I was young, I've gravitated toward going to sleep late. Even as an 11-year-old, I relished that I had my own room where I could crash at midnight after reading. Gradually, as I got older, my bedtime went later and later. In high school, it was about 2 a.m. because of endless homework. When I got to university, I threw caution to the wind and regularly went to sleep between 3 and 5 a.m.
When I got an internship at a traditional 9-to-5 workplace in the city, I would force myself to sleep at 2 a.m., just so that I'd get at least five hours of sleep per night. When the internship ended, my sleep cycle bounced back to my regular 3 to 5 a.m. During the pandemic, it got even later.
After years of taking melatonin and trying every natural sleeping medication for what I assumed was insomnia, I decided to talk to my doctor and was finally diagnosed with delayed sleep phase syndrome.
What is delayed sleep phase syndrome?
Delayed sleep phase syndrome (DSPS)—also known as delayed sleep phase disorder (DSPD) or delayed sleep-wake phase disorder (DSWPD)—is a condition where a person's sleep is delayed by two or more hours beyond what is generally considered a "normal"' bedtime. The delayed sleep causes trouble with waking up, particularly for school and traditional workplaces.
Unlike being a night owl, people with DSPS don't choose to go to sleep late. Instead, it just comes naturally to us, impacting our work and social and family life.
Delayed sleep phase syndrome is a type of circadian rhythm sleep-wake disorder (CRSWD). The circadian rhythm is the internal process that regulates our sleep-wake cycle. According to the International Classification of Sleep Disorders, circadian rhythm sleep-wake disorders must meet three major criteria for diagnosis.
- Chronic or recurrent patterns of sleep-wake rhythm disruption primarily caused by an alteration in the endogenous (i.e., not externally influenced) circadian timing system or misalignment between the endogenous circadian rhythm and the sleep-wake schedule desired or required.
- A sleep-wake disturbance, such as insomnia or excessive sleepiness.
- Associated distress or impairment. For all CRSWDs, except for jet lag disorder, a duration criterion of at least three months has been added.
Where does DSPS come from?
Some scientists suggest DSPS may result from a genetic mutation, but many factors could be at play. Dan Ford, a sleep psychologist at The Better Sleep Clinic in Auckland, New Zealand, offers an evolutionary explanation.
"From an evolutionary standpoint, a tribe would do well to have members awake throughout the night for collective protection so different body clocks can help ensure this happens," Ford said. "There is speculation it's helpful for teens to have a delayed sleep phase to help them separate from their parents, connect with each other and begin their journey to maturity."
There has also been evidence linking DSPS and attention deficit hyperactivity disorder (ADHD), with about 73-78 percent of ADHD adults and children also having DSPS.
Researchers found that modified circadian rhythms in ADHD individuals may be due to a dysfunction of the locus coeruleus. It is a region at the back of the brainstem close to the cerebellum, involved in the onset and offset of rapid eye movement (REM) sleep. In people with attention deficit hyperactivity disorder, the arousal processes of the locus coeruleus may be impacted.
Chelsie Rohrschieb, M.D., is the head sleep specialist and neuroscientist for Wesper, a sleep, wellness and tech company. Over the years, her research in the sleep medicine field has supported this connection.
"Studies found individuals with ADHD had physically smaller pineal glands, an area of the brain that is responsible for producing the circadian rhythm-regulating hormone, melatonin," Rohrschieb said.
This effect may be worsened by the treatment of attention deficit hyperactivity disorder, which often involves stimulants that can cause insomnia and difficulty falling and staying asleep at night, especially if the stimulants are taken later in the day.
However, Ford warns of a different possible vicious cycle.
"The behavioral and cognitive consequences that arise in DSPS because of excessive daytime sleepiness can look like behaviors characteristic of ADHD," he said. "So there is a risk of misdiagnosis going in both directions. You may be more likely to see DSWPD in conditions such as insomnia, depression and anxiety."
Ford also points out there is evidence indicating more intangible risk factors.
"Personality factors can contribute to delayed sleep phase syndrome with research suggesting DSPS is associated with higher neuroticism and significantly lower extraversion, conscientiousness and agreeableness," Ford said.
If you feel you may have delayed sleep phase syndrome, it might be time to seek help from a specialist and get evaluated.
Getting diagnosed
Ford recommended seeking treatment if you can check any of the following boxes:
- Difficulty falling asleep more than three nights a week for more than three months.
- Failing to meet obligations because you can't wake up in the morning.
- Excessive daytime sleepiness because of your lack of sleep.
Ford also says it's also an issue if you experience any of these problems and yet can fall asleep and stay asleep when you can choose your own schedule.
Sleep diaries and interviews with your doctor help with the diagnosis. Your doctor may also use a sleep study test, known as a polysomnography, which records your brain waves, blood oxygen, breathing and heart rate, and leg and eye movements while you sleep.
Although most often conducted at a hospital or sleep clinic, many polysomnographic tests can now take place in the comfort of your own home. In some cases, they may conclude in a diagnosis of sleep apnea, which can secondarily disrupt the circadian rhythm.
However, if you're diagnosed with delayed sleep phase syndrome, it's time to start treatment.
Treating DSPS
For Ford, treatment often includes bright light therapy.
"The treatment is timed bright light and strategically timed melatonin administration," Ford said. "It is an effective treatment and quick to shift a patient's circadian rhythm to a more socially desirable sleep period. However, that patient will always be at risk of their body clock drifting back to its preferred timing and will have to manage their body clock throughout their life."
He also added Cognitive Behavior Therapy for Insomnia (CBTI) is an effective treatment for any residual insomnia symptoms that result from DSPS. This form of treatment works by helping us identify thoughts, behaviors, feelings and actions that contribute to insomnia. A practitioner will then try to reshape those conceptions and challenges in a way more conducive to sleep. Treatment can take anywhere between 6-8 sessions.
CBTI includes three main processes:
- Cognitive interventions, which restructure unhelpful thoughts surrounding sleep.
- Behavioral interventions, which include relaxation training and sleep restriction to promote healthy sleep habits.
- Psychoeducational interventions—sharing information about the relationship between feelings, thoughts, behaviors and actions surrounding sleep.
A sleep psychologist often conducts CBTI. However, there are virtual options such as CBTi-Coach from the Department of Veterans Affairs and the Simple Habit meditation app as well. Workbooks and handouts such as this could also prove effective and affordable for monitoring and changing your sleep cycle at home.
As for pharmacological treatments, prescription sleep aids can help with resetting your sleep cycle and falling asleep at an earlier time, plus over-the-counter supplements and vitamins can aid with sleep.
Leigha Saunders, ND is a naturopathic practitioner in Ontario, Canada who often works with patients suffering from DSPS, and recommends several everyday adjustments.
"Wearing blue light-blocking glasses in the evening can help to limit your exposure to blue light, which decreases your overall production of melatonin," Saunders said. "Conversely, exposing yourself to blue-light (natural sunlight is best!) in the morning can help decrease melatonin production and help you feel more awake."
Saunders cited a small study of eight patients who experienced earlier melatonin production and earlier sleep after wearing blue light-blocking glasses from 9 p.m. onward for two weeks.
If all else fails—including sticking to good sleep hygiene habits—and your sleep cycle remains nocturnal, Ford said it may be time to change your lifestyle altogether.
"DSPS individuals are particularly well suited to night-shift work," Ford said. "But as shift work is not overly great for any human, I'd suggest jobs where you can choose your hours."

















