CDC Updates Pain Management Guidelines for IUD Insertion and Removal

Key Points
- IUD insertion and removal isn't always painful, but it can be.
- Until now, many healthcare providers haven't routinely offered patients pain management options, such as lidocaine as a cervical block or topical gel, cream or spray.
- The CDC issued new guidelines stating that providers should inform patients about the potential for severe pain and give them various management choices.
Folks on TikTok have long been angry over the lack of sedation for those getting or removing IUDs (intrauterine devices). Now, it appears as though the medical community is starting to listen.
The Centers for Disease Control and Prevention (CDC) released new 2024 guidance acknowledging that these procedures can be painful—and advising physicians to do more to help patients prepare. It's the first update since 2016.
What are the new CDC guidelines for IUD insertion and removal?
Earlier this month, the CDC issued the U.S. Selected Practice Recommendations for Contraceptive Use, 2024, which includes advice to physicians inserting or removing hormonal or copper IUDs.
The new recommendations say practitioners should do more before IUD procedures to counsel patients on the potential for pain and ways to manage it. Additionally, the updated guidance urges providers to recognize that some patients might find the procedure more painful than others.
"When considering patient pain, it is important to recognize that the experience of pain is individualized and might be influenced by previous experiences including trauma and mental health conditions like depression and anxiety," the new guidelines say.
The updated guidance recommends offering patients several options to manage pain and stress during the procedure, such as oral pain relievers, local anesthetics or anti-anxiety medications.
One of the options includes lidocaine, which can be administered as a cervical block via an injection or as a topical gel, cream or spray. Previously, the CDC only recommended lidocaine injections, which can be painful.
Practitioners can also consider providing misoprostol to certain patients, such as those who have cervical scarring or recently had a failed IUD placement, according to the updated guidelines.
"I am hopeful that the medical community will continue to make up for lost time related to improving understanding of and care for women. It is well known that research and funding related to women's health has not been prioritized," said Allison Salk, M.D., an OB-GYN with Rush University System for Health in Chicago.
"I feel grateful to be in this field during a time when women's health is getting more attention. I hope that this decision is one of many decisions that emphasize evidence-based, patient-centered health care related to women's health," Salk said.
Why were people angry that getting or removing an IUD doesn't involve sedation?
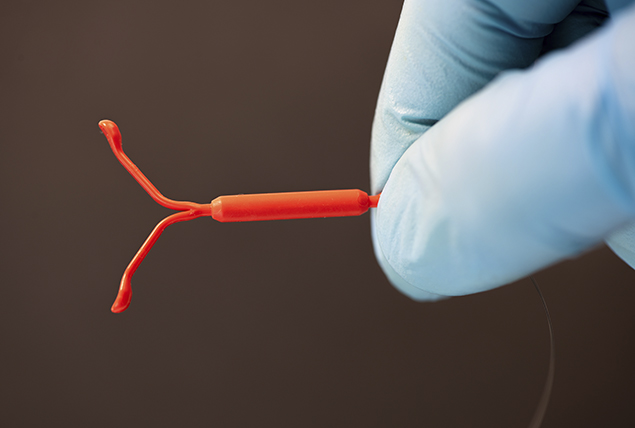
First, let's do a quick rundown on what an IUD is. An intrauterine device is a T-shaped plastic device placed in the uterus to prevent pregnancy. There are two types of IUDs, a copper IUD and a hormonal IUD.
A copper IUD has a metal coating that repels sperm, while hormonal IUDs release the hormone progestin to prevent ovulation and thicken cervical mucus to stop sperm from reaching an egg.
When placed before sex, they're more than 99 percent effective at pregnancy prevention. IUDs can also be used to help manage heavy periods or within 120 hours of sex as a form of emergency birth control.
"Some people only report having discomfort, not pain, with IUD insertion or removal," Salk said.
Others, however, report severely painful, stressful experiences. Many of the latter have shared their stories online and expressed frustration or anger that they weren't offered better pain management options.
"With the invention of social media and TikTok, I believe patients now feel empowered to share their personal experiences in a way we have never seen before. This is wonderful. Patients can connect with others over a shared experience and create a community on social media," Salk said.
"However, for some patients, watching videos and hearing stories of painful IUD experiences may increase their anxiety when they choose to have an IUD placed."
Recommended
- What Should You Know About Birth Control on Your College Campus?: Student health plans offer a range of contraceptive methods; off-campus options exist.
- Progestin-only Pills May Be More Effective Than Previously Believed: A new study suggests the minipill could be 98 percent effective with typical use.
- At What Age Can You Get a Vasectomy?: All aspects of this life decision should be considered, including how old you are.
Salk noted that this makes it even more important for doctors to educate patients and ensure they feel comfortable and well-prepared.
"They should know that every IUD insertion is different and that we hope to tailor their experience to best suit them with the options that we have available for pharmacologic and nonpharmacologic pain management options," she said.
Healthcare providers don't always acknowledge that the procedure could prove painful. Research reveals healthcare providers often underestimate patients' pain levels during IUD insertion or removal and other gynecological procedures.
On average, women rate their IUD insertion pain at 64.8 mm on a 100-mm visual analog scale, while healthcare providers rated patients' pain at 35.3 mm, according to a 2014 report.
"Extensive, rigorous research on IUD insertion pain management has only occurred within the last decade or so," Salk said. "Therefore, there were not as many standard guidelines on pain management during IUD insertion, and practices varied from office to office."
Why would IUD insertion or removal necessitate anesthesia?
An intrauterine device is inserted and removed by way of the vagina through the cervix. Your gynecologist will use a speculum—the same tool used in pap smears—to access the cervix.
A tenaculum is then used to hold the cervix in place while measuring the depth of the uterus and inserting or removing the IUD.
"There are no cuts or incisions, but pain or discomfort can occur as the IUD is inserted when the instrument is placed inside. The uterus may also have cramping when it is measured as part of the insertion process," Salk said.
The bottom line
The process of IUD insertion or removal can be painful. However, as one of the most effective forms of birth control, it's a worthwhile consideration for many.
If you're anxious about getting your first IUD or having it removed, talk with your healthcare provider about the pain options available. They can provide a recommendation based on your preferences and needs.