Annual PSA Screenings Show Benefits for Black Men, Study Finds

The use of prostate-specific antigen (PSA) screening may be beneficial for Black men, a recent study found. That's despite some medical bodies recently deemphasizing the test or even recommending against it.
The research examined the association between PSA screening and prostate cancer-specific mortality (PCSM) among Black and white U.S. veterans. The findings showed a reduced risk of PCSM among Black veterans who received annual PSA screenings, but not among their white peers.
These findings are particularly important because researchers used data from the Veterans Health Administration (VHA), where all veterans have equal access to care. That is not always the case outside of the military.
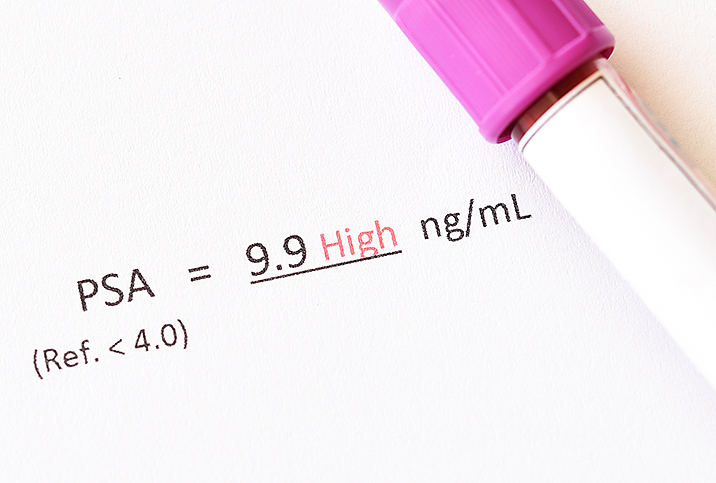
The PSA test
The PSA screening test uses a blood sample to screen for prostate cancer. It has its proponents and detractors and has seen its popularity rise and fall. This study may boost its implementation, at least for Black men.
"PSA is a protein produced by the prostate by both cancerous and noncancerous tissue, hence, PSA can rise in both benign and cancer situations. In most situations, urologists use PSA as well as other diagnostic tools to diagnose prostate cancer," said Justin Houman, M.D., a reproductive urologist and men's health specialist at Tower Urology in Los Angeles and the medical director for Bastion Health, an app-based telehealth platform for men. "Rising PSA is concerning and warrants further investigation, sometimes in the form of prostate imaging and prostate biopsies."
The protein is secreted by other body parts outside of the prostate, too. Certain conditions such as a recent illness or catheterization can also result in increased PSA production, according to Denise Asafu-Adjei, M.D., an assistant professor of urology and the medical director of male reproductive medicine at Loyola University Chicago Stritch School of Medicine.
What the study shows
The cohort study used data from 45,834 U.S. military veteran participants, of whom 31 percent identified as Black and 69 percent as white. It highlighted that while Black men have a higher prostate cancer incidence and mortality rate, they've been underrepresented in PSA screening trials, leading to a lack of data to provide proper recommendations.
The research was based on data from the VHA Informatics and Computing Infrastructure for men identifying as Black or white, ages 55 to 69, with a diagnosis of intermediate-, high-, or very high-risk prostate cancer between 2004 and 2017. The average age of the participants was 62.7.
The study authors used Fine-Gray regression analysis, a model that estimates the prevalence of outcomes over time in the sight of competing risks to assess any association between PSA testing and the risk of PCSM. The risks were also assessed by the frequency of previous PSA testing among participants, categorized as:
- No prior PSA screening
- Some screening
- Annual screening five years prior to cancer diagnosis
The study reported a lower risk of PCSM among both Black and white men who had PSA screening. However, annual screening had a significant reduction in PCSM risk among Black men, but not among white men, compared with less frequent screening.
The research concluded that annual PSA screenings may be particularly important for Black men. Further research, though, "is needed to identify appropriate populations and protocols to maximize the benefits of PSA screening," the study authors wrote.
"PSA [screening] itself is not more beneficial for African American men," Asafu-Adjei said. "However, African American men have more aggressive forms of prostate cancer, so screening is especially important in this higher-risk population."
Houman added that about 1 in 6 Black men are diagnosed with prostate cancer.
"Prostate cancer is also more common in Black men than other ethnic groups. Finally, prostate cancer is deadlier in Black men as it has a different genetic profile, thus, making it a more aggressive cancer at diagnosis," he said.
The ups and downs of annual PSA screenings
According to the National Cancer Institute, in 1986, the U.S. Food and Drug Administration (FDA) authorized PSA screening to monitor the progression of prostate cancer. Eight years later, it further approved PSA testing as a form of prostate cancer detection in men ages 50 and older.
PSA testing was highly encouraged by doctors and organizations until about 2008. After learning more about the benefits and potential harms of screening, medical organizations began to caution against the test. They advised patients to discuss the advantages and side effects of the process, and the reliability of the potential results, with their doctor. They recommended it for men who are at higher risk of developing prostate cancer.
The U.S. Preventive Services Task Force (USPSTF) updated its recommendation for PSA screening in 2018. It does not recommend PSA screening tests for men ages 70 and older. Men ages 55 to 69, however, should be given the choice to undergo periodic PSA screening after careful discussion and consideration of the potential benefits and harms with their clinician.
"PSA screening is not without risks, including unneeded prostate biopsies, anxiety over potential cancer diagnoses and overdiagnosis of prostate cancer," Houman said.
PSA testing is not recommended in the United Kingdom, according to the National Health Service (NHS). Men who inquire about the screening with their general practitioner can be tested and the NHS will cover the cost.
"It has not been proved that the benefits would outweigh the risks," said an NHS statement. Instead, it recommends an MRI scan before a biopsy to help avoid any further unnecessary examinations.
As is always the case, PSA screening or not, talk to your doctor if you have any questions or concerns about prostate cancer.