Are 'Acne Bumps' Something You Should Worry About?
Board-certified dermatologist Gibran Shaikh, M.D., explained that hidradenitis suppurativa (HS) may be known by its more familiar name, acne inversa.
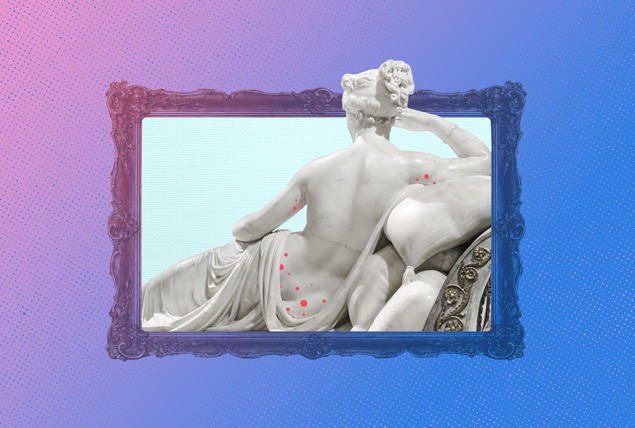
"It's a chronic inflammatory condition characterized by inflammation of the skin, in which people get these deep abscesses, which are collections of pus, predominantly under their arms and the genital region, in the breast area and buttocks," said Shaikh, who is based in New York City.
In other words, it can be visually conceptualized bluntly as an "acne bump," he said. Although the disease tends to afflict people of color, white people also can be affected. Still, it generally affects people with darker skin types, as evidenced by several extensive epidemiological studies.
"Why that is, is unclear," Shaikh said. "It could be that white individuals are getting care at an earlier stage and it prevents progression because they have better access to care. But, on the other hand, it could represent genetic differences."
Although the disease does not have a strong predisposition to gender, he said women are more likely than men to seek care earlier. Men are more likely to suffer from the problem silently, even though early treatment is critical to preventing its symptoms.
Areas of the body with high friction are most commonly associated with hidradenitis suppurativa, which follows the pattern of acne-related skin conditions.
How your sex life can be affected
Shaikh suggested imagining yourself in the shoes of a person with hidradenitis suppurativa.
"You have draining sinuses filled with pus, and maybe there's a bad smell," he said. "Obviously, there's going to be some aversion toward intimacy or baring one's body in front of an intimate partner."
His patients report self-esteem issues due to the symptoms, which naturally hinders their confidence and sex life. Potential partners may not understand this condition is not contagious or confuse it with a sexually transmitted infection (STI). It's vital to seek early diagnosis and treatment to prevent the disease from worsening and negatively impacting your mental health.
Beyond stigma, Shaikh said his patients report physical pain, because the condition can affect sensitive areas such as the groin. The lesions can be extremely painful, particularly when they're actively inflamed.
"Additionally, many patients with hidradenitis also have coexisting depression and anxiety, or maybe substance use issues," he added. "They may be on medications, for example, for depression, partly because of HS that's causing them to be depressed, and those medications also cause sexual dysfunction."
Shaikh said a combination of factors ultimately come into play on the overall impact hidradenitis has on a person's health and sex life. Seeking a diagnosis and treatment should be the first step to coping.
Learning how to communicate information about the disease and its symptoms to your partner is another actionable step to normalcy and can be done through your healthcare provider or by contacting the Hidradenitis Suppurativa Foundation for available resources.
Navigating life after diagnosis
Steve Daveluy, M.D., associate professor and program director of the Wayne State University Department of Dermatology in Detroit, pointed to studies indicating that hidradenitis suppurativa significantly impacts a patient's life compared with other skin diseases such as psoriasis and eczema, especially in regard to sexual health and intimacy.
He added that educating experts on the disease and providing them with tools to help their patients is a crucial step.
"It's really important to receive a diagnosis and start a treatment plan with a board-certified dermatologist skilled in treating HS," Daveluy explained. "While it can take some time to find the right treatment regimen to control the disease, it greatly benefits mental and sexual health when you do. If you have boils or pimples that come and go in your armpits, groin, buttocks or under the breasts, you most likely have HS and should see a dermatologist."
Don't keep struggles to yourself
Daveluy noted that if you aren't sure but think you may have hidradenitis, the website of the American Academy of Dermatology has excellent information to help you in your journey. Beyond treating its physical symptoms, though, visiting with mental health professionals—particularly sex or intimacy therapists—can be a powerful resource for regaining control of your life.
Counseling and support groups are available. There are anonymous health groups and forums online where patients may feel more comfortable discussing issues like this condition.
"Hidradenitis suppurativa can also make you feel isolated and alone," Daveluy said. "Connecting with other patients through online patient groups is something I recommend to all my patients with HS. Hope for HS and HS Connect are great options, and other patients often share their tips and life hacks for living with HS."
He recommended that anyone suffering in silence should talk to their doctor, dermatologist, partner, other patients and/or mental health professionals.
"Don't be shy or embarrassed to share that you're struggling with intimacy," Daveluy added. "It's just a part of your health."
The silver lining starts when you take advantage of the resources in front of you. Daveluy said he has many hidradenitis suppurativa patients who lead happy lives filled with intimacy.
"Some are well-controlled with our treatments," he noted. "There are others where we're still trying to get things under control, but they have found ways to thrive in their intimate relationships."
The most important strategy is to not give up hope. Hidradenitis suppurativa is not the end of intimacy or your sex life. But it might give you a new appreciation for how good it can be. Every health struggle you overcome can only make you more attuned and aware of your body, and you'll end up stronger.


















