Osteoporosis Is a Serious Concern After Menopause

Osteoporosis disproportionately affects biological women, particularly those of menopausal age. Of the 10 million people age 50 and older in the United States who have osteoporosis, about 80 percent are women, according to the U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion.
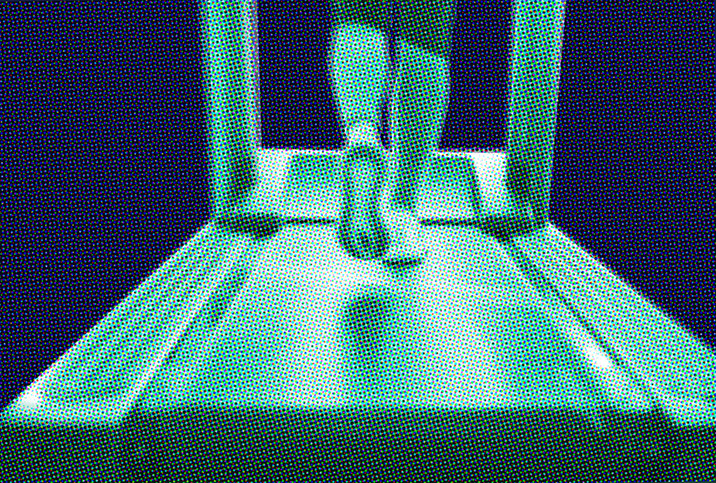
Osteoporosis, which means "porous bones," occurs when bone mineral density and bone mass decrease, making bones weak, brittle and more susceptible to fractures. It is known as a "silent" disease because it's often asymptomatic in the early stages.
"Often, the first symptom is a broken bone," said Alyssa Dweck, M.S., M.D., a Westchester County, New York-based OB-GYN and chief medical officer at Bonafide, which creates women's health products.
Other symptoms can include back pain, often resulting from a collapsed or fractured vertebra, stooped posture and gradual height loss.
The impact of osteoporosis
People with osteoporosis can experience spontaneous fractures with no discernible trauma. Bones affected by osteoporosis can also break due to minor stresses, such as bending, lifting or falling from a standing position, that wouldn't usually cause severe harm.
About 1 in 2 women older than age 50 experience an osteoporosis-related fracture, according to the Bone Health & Osteoporosis Foundation (BHOF).
"A broken hip, leg or even wrist can be debilitating," Dweck said.
In addition to inhibiting a person's ability to work or participate in day-to-day activities, these injuries can have a long-lasting negative impact on quality of life and increase the risk of chronic conditions, including pain and arthritis.
Evidence also indicates a correlation between osteoporosis-related fractures and mortality, especially in the year following an injury. A 2011 investigation published in JAMA Internal Medicine found hip fracture cases had twofold increased mortality in the year after fracture compared with control participants.
The researchers concluded that short-term mortality is increased after hip fracture in women ages 65 to 79 and in exceptionally healthy women 80 years or older. Women 70 years or older return to previous risk levels after a year.
The link between osteoporosis and menopause
Menopause indicates the end of a person's menstrual cycles and fertility. It's diagnosed after a person has gone without a period for 12 months and usually occurs in a person's 40s or early 50s, though it can happen earlier or later.
Although it is a natural biological process, menopause can have adverse effects, including hot flashes, fatigue, sleep disruptions, increased fat and decreased muscle mass, anxiety, vaginal dryness, cognitive changes, increased risk of heart disease and osteoporosis risk. Most of these effects occur because of dramatic changes in hormone levels, mainly decreased estrogen and progesterone.
Estrogen is a hormone primarily produced in the ovaries, though fat cells and adrenal glands produce some, as well, explained Brynna Connor, M.D., an Austin, Texas-based physician and healthcare ambassador at Northwest Pharmacy.
Although its primary function is reproductive system development and maintenance, estrogen also plays a key role in bone, breast and brain health, Connor said. Estrogen bolsters bone strength, and the lack of it can contribute to weak, brittle bones and osteoporosis.
Bone is living tissue that is routinely broken down and replaced, explained Michelle Swer, M.B.B.Ch., M.R.C.O.G., consultant gynecologist for London Gynaecology at the Portland Hospital in London. New bone develops more rapidly than old bone breaks down in the first half of life, increasing overall bone mass.
"The process of bone remodeling is affected by several hormones, including estrogen," Swer said. "Estrogen plays an important role in promoting the activity of the cells that are responsible for making bone. At menopause, estrogen reduces, which affects the normal bone turnover cycle, leading to more bone being broken down than being increased."
According to Connor, the most marked loss in bone mineral density occurs during the 12 months before a person's final period and the first two years afterward.
"Menopause is the most important risk factor for bone density loss in women in the perimenopause and early menopausal age ranges," Connor explained. "Women can lose about 30 percent or 50 percent of their cortical [external layer] and trabecular [porous] bones, respectively, throughout their lives, and half of that bone loss typically occurs in the first decade after menopause begins."
Bone density continues to decrease with time, Swer said. However, after the first decade of menopause, the reduction is primarily age-related, as both men's and women's bodies produce less new bone in senior years.
Risk factors and prevention
In addition to menopause and age, several other factors can increase a person's risk of developing osteoporosis. According to Dweck, Swer and Connor, these factors include:
- Being a biological woman
- Being white or Asian
- Family history of the disease
- Being petite or thin
- Smoking
- Heavy alcohol use
- Sedentary lifestyle
- Diet low in calcium or vitamin D
- Thyroid or parathyroid disorders
- Inflammatory bowel disease (IBD)
- Celiac disease
- Rheumatoid arthritis
- Early-onset menopause
- Use of steroid medications
- Eating disorders or another medical issue causing lack of menstruation for over a year before menopause
As with many medical conditions, taking proactive measures early on is the best way to decrease the risk of osteoporosis.
"Healthy diet, exercise and lifestyle choices throughout life will limit bone density loss and decrease osteoporosis risks during menopause," Connor said.
In addition to eating a balanced diet and maintaining a generally active, healthy lifestyle, Dweck, Connor and Swer stressed the importance of getting sufficient calcium and vitamin D, essential nutrients for bone development and maintenance.
The recommended doses are 1,200 milligrams of calcium and 800 to 1,000 international units of vitamin D3 per day for most people. Natural sources are best for calcium and vitamin D, though supplements can help. Remember, you should always consult your doctor before adding a supplement to your diet to make sure the dosage is correct for your individual needs.
When choosing a type of exercise in midlife and beyond, experts recommend weight-bearing activities, such as walking, weightlifting, jogging or stair climbing, to support bone strength and flexibility, and balance training to reduce the risk of falls.
Treating osteoporosis
If you develop osteoporosis, Connor advised continuing to make healthy lifestyle choices to slow the disease's progression and reduce the risk of fractures.
"Prevention is ideal, but both oral and injectable medications are available for the appropriate candidates," Dweck said. "I typically suggest a consultation with an endocrinologist to address this and review options."
One medication option is bisphosphonates. This type of drug can slow osteoporosis advancement, increase bone density and, according to a 2017 study published in the Journal of Bone Metabolism, reduce the risk of overall osteoporotic fracture. Another bone-loss prevention treatment is monoclonal antibodies.
Menopausal hormone therapy (MHT) may also help prevent osteoporosis but is not considered a first-line treatment.
"But when balancing risks and benefits on an individual basis, [MHT] has been found to increase bone density mass and can, therefore, be indicated when women are suffering from other menopausal symptoms," Swer explained.
If you are worried about osteoporosis risk during your menopausal transition or postmenopausal years, don't wait—speak with your doctor today for testing and treatment options.