Manage Persistent Pain With Help Beyond Medication

If you're reading this article, you may be familiar with the constant challenges of living with chronic pain. Sometimes even routine tasks, such as walking, climbing stairs, carrying groceries, picking up your child or sexual activity, may be a struggle.
The challenges posed by chronic pain can erode a person's sense of happiness and well-being, as well as cause relationship issues if sexual health declines. And sometimes taking a pill for pain isn't enough or isn't an option.
More than 20 percent of U.S. adults suffer from chronic pain, which translates into more than 50 million people reporting symptoms and seeking treatment. About 7 percent of U.S. adults live with high-impact chronic pain, which severely restricts their lives at home and work.
Researchers and doctors want to reclassify chronic pain as a disease in hopes of unifying health policies and creating better treatment protocols.
In the meantime, people suffering from chronic pain are actively looking beyond traditional Western medicine in search of other pathways to relief.
Alternative pain management
Tenley Fukui, M.A., L.P.C., has a master's degree in clinical psychology and is certified in clinical hypnosis by the American Society of Clinical Hypnosis. She provides individual therapy both in person in Houston and via telehealth.
"According to the International Study of Pain's latest definition, pain is an unpleasant sensory and emotional experience that is associated with actual or potential tissue damage," she explained. "Pain is also a personal experience influenced by biological, psychological and social factors."
Chronic pain exposes clients to pain for extended periods of time, which means "beyond normal tissue healing time, usually 12 weeks, and [is not] responsive to treatment," Fukui continued. "However, people can be taught how to manage it to an acceptable level. For over 20 years, pain clinics and chronic pain specialty providers [have] offered a biopsychosocial approach in multidisciplinary pain management programs."
The role of hypnotherapy
"Hypnosis is a state of mind where you have very focused attention," Fukui said, adding that a common example of hypnosis is daydreaming. While in this relaxed state, people are more open to suggestions, Fukui explained. A person may experience burning back pain, and with hypnosis the pain can be changed to a cooler sensation, perhaps by suggesting the feeling of an icy mountain stream on their back.
Research indicates that "hypnotic analgesia—and treatments containing hypnotic elements such as progressive muscle relaxation—decrease many types of pain [and] outperform non-hypnotic treatments such as education and supportive therapy," she added.
These positive responses from hypnotherapy treatments stem from the intricate communication pathways between our brains and bodies, referred to as the pain gating system.
"If your [arm] accidentally touches something hot, the pain signal travels up your arm, through the pain gating system in your spinal cord to your brain," Fukui said. "Your brain identifies this signal as 'uncomfortable' and sends the signal back down your spine for you to [remove] your arm from the heat. This signal can be modified from the gating system in your spine. For example, a positive mood, a distraction [or] deep, relaxed breathing can close or partially close [the] pain gate, while strong emotions such as fear, anxiety and thinking the worst can open the pain gate."
The mechanism of how hypnosis works for pain management is thought to be related to altering or influencing this pain gating system through suggestions made by the therapist during hypnosis.
A naturopathic doctor's approach to pain
Practicing in Nova Scotia, Tara Lapointe, N.D., B.Sc.H., a licensed naturopathic doctor and registered yoga teacher, described her approach as "to help find and treat hidden causes of inflammation that may be contributing to that perfect storm of root-cause factors setting off the chronic pain cycle, while also rewiring the nervous system in order to process the pain differently."
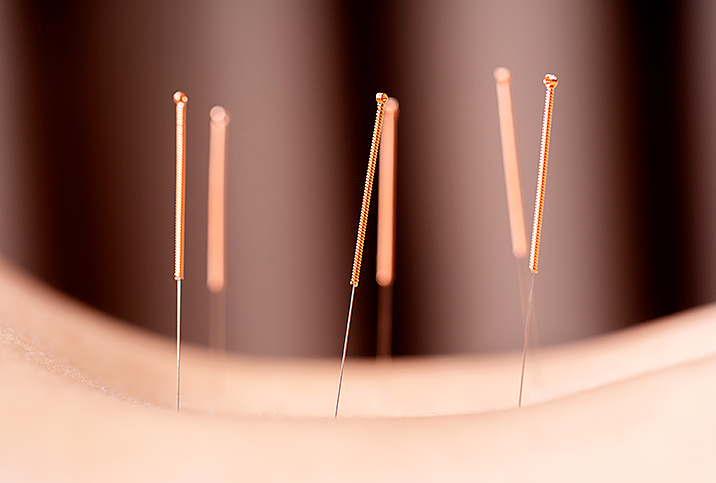
"Traditional allopathic medical models focus on treating the pain itself with analgesic treatments," she said. "This is very helpful in the short term but does not look into the root causes of the pain. In the long term, many of the treatments for pain cause dependency and come with many potential serious side effects. Incorporating [other] therapies into pain management—such as physiotherapy, acupuncture, massage therapy, osteopathy, to name just a few—helps to work on the root causes [and] aid with pain management."
This "rewiring process" using naturopathic protocols "can be as simple as learning novel distractions such as breathwork, hydrotherapy or taking up a new hobby," Lapointe added. "In my practice, along with lifestyle modifications and supplement suggestions, I incorporate yoga nidra, acupuncture and PEMF [pulsed electromagnetic field] therapy sessions to reset the nervous system."
Whole person pain management
During Fukui's internship with the pain clinic at the Michael E. DeBakey Veterans Affairs Medical Center in Houston, she worked with an interdisciplinary medical team.
"I led psychotherapy educational pain groups and offered individual pain psychotherapy," she explained. "I also developed and ran a pilot study for treating veterans with chronic low back pain. This study revealed that veterans had decreased lower back pain and improved sleep."
A subsequent randomized controlled trial revealed that two sessions of self-hypnosis with audio recordings may be as effective for pain reduction as eight sessions, with or without recordings or biofeedback therapy.
In addition, all hypnosis groups displayed better pain relief than the biofeedback control group. This is good news for people who have limited time for treatments that could be carried out via telehealth.
Biofeedback therapy involves connecting electrical sensors to your body to monitor information, allowing you to make subtle changes such as muscle relaxation. The goal of the therapy in this case was to reduce pain.
Fukui also uses biofeedback in her practice.
"Most clients find it helpful to see their EMG biofeedback muscle tension on a computer screen to learn how to decrease neck tension, for example, which can cause headaches," Fukui said.
According to Fukui, during biofeedback therapy—whether the patient is in hypnosis or not—this information gives the client a window into how their body experiences pain and/or stress. For example, their temperature may rise, showing increased relaxation, or their temperature may decrease, indicating increased anxiety or stress, she added.
Seeing patients beyond their symptoms and individualized treatments are essential in both hypnotherapy and naturopathy.
"In many cases, no physical causes for pain are identified," Lapointe said. "People react much differently to the same painful procedures, such as a blood draw, highlighting that there is a huge cognitive and emotional component to the experience of pain."
This experience makes sense given that pain lights up the same area of the brain associated with isolation, depression and stress, she added.
Becoming a medical investigator
"As humans, we love tidy, simple equations of X equals chronic pain, however, in reality there are plenty of ingredients stewing together to make the perfect storm [of] X plus Y minus Z times A equals pain," Lapointe said. "For many patients, the experience of pain is often multifactorial, which may be a combination of acute and chronic factors that lead to inflammation and pain perception.
"Some examples include old injuries, autoimmune diseases and poor biomechanics," Lapointe continued. "Environmental toxins, inflammatory foods, gut dysbiosis, nutritional insufficiencies and hormonal dysregulation can also cause inflammation."
Lapointe outlined a few dietary and lifestyle changes that may aid pain relief. Find reputable sources for any supplements you add to your daily regimen, but first discuss any changes to your diet with your healthcare provider.
- Intermittent fasting. "Eating a whole-food diet low in sugar and processed food is key. But adding in an extended fast overnight anywhere from 12 to 16 hours allows the body to rejuvenate," Lapointe said.
- Turmeric. "This spice is a versatile, natural anti-inflammatory. The active component curcumin is found in supplement form, but for general support, you can use turmeric in cooking or as a latte with one-fourth teaspoon of each turmeric, ginger, cinnamon and a pinch of pepper, vanilla extract, all in warmed almond milk with a touch of honey," she said.
- Fish. "The omega-3 oils in fatty fish are a great anti-inflammatory. You can get these in a supplement form or focus on eating more of the SMASHT—salmon, Atlantic mackerel, anchovies, sardines, herring and trout—fish in your diet," Lapointe said.
- Breathing. "Breathing can positively affect our heart rate variability [HRV] and the increase and decrease of our heart rate as we breathe in and out. A better HRV is associated with better health, including reductions in pain perception," Lapointe said. "A quick HRV reset exercise involves focusing on breathing in and out of the heart area of the chest: breathing in relaxed and slowly for a count of four and out for a count of four as you think about a loved one, a beautiful place or an accomplishment you're very proud of. One minute of this exercise can drastically improve your HRV."
- Cold plunges. "Cold water therapy is known to reduce inflammation, alter pain perception and increase neurotransmitters and endorphins. Care should be taken to make sure you approach this slowly and under the guidance of an experienced professional. This can be as simple as daily cold showers and as extreme as ice swimming," she said.
Lapointe recommended consulting your primary care provider before making any changes to your overall healthcare routine.