Detecting STD Symptoms as Their Rates Climb

In 2021, the Centers for Disease Control and Prevention (CDC) reported that sexually transmitted diseases (STDs) climbed to an all-time high for the sixth consecutive year, from 1.9 million new cases in 2014 to more than 2.6 million in 2019. With numbers on a sharp upward trend, are you at risk of contracting an STD and can you recognize STD symptoms?
STDs spread in one of two ways, said Pippa Murphy, a sex and relationship expert at online retailer Condoms.uk in the United Kingdom:
- Certain diseases, such as gonorrhea, chlamydia and HIV, are passed on through infected secretions from the vagina or penis coming into contact with mucosal surfaces, such as the cervix, vagina or urethra.
- Other diseases, such as genital ulcer diseases like syphilis, chancroid, genital herpes and HPV, are transmitted when infected skin or mucosal surfaces come into contact.
Monte Swarup, M.D., a board-certified OB-GYN in Arizona and founder of HPV Hub, stressed that different STDs have different symptoms. There is no one set of symptoms that fits all STDs, and it's important to note that some diseases—for instance, the monkeypox virus—may have sexual modes of transmission without being STDs.
Common signs and symptoms of STDs
Murphy described five of the most common STDs:
Syphilis
Syphilis is a bacterial infection passed on through oral, anal or vaginal sex. Skin-to-skin contact can transmit syphilis. One of the initial symptoms of syphilis is a sore, known as a chancre, which develops around the infected site.
Other symptoms include:
- Additional ulcers and sores around the genitals, anus or mouth
- A red rash covering the soles of the feet or palms of the hands
- Skin growths that look like genital warts appearing around the vulva or anus (for men and women)
- White patches in and around the mouth
- Tiredness
- Joint pains
- Headaches
- Fever
- Swollen gland in the armpits, neck and groin
Swarup added that syphilis has different symptoms at different stages as follows:
- Primary. Syphilis appears as a painless chancre, which goes away in three to six weeks without treatment.
- Secondary. If syphilis is left untreated, a rash may appear on the soles of the feet and palms of the hands after having the chancre. Flat warts may appear on the vulva, and flu-like symptoms are possible.
- Latent infection. While the infection remains in the body after the rash, other symptoms may go away in a few weeks or months.
- Tertiary. This stage may occur some 10 to 30 years after initial infection and affects the heart, blood vessels, brain and nervous system. Symptoms include problems controlling muscle movements, numbness, vision issues and dementia. Such effects could result in death.
Herpes
Herpes is caused by the herpes simplex virus (HSV) and passed on through vaginal, oral or anal contact with a partner. The virus causes sores around the mouth, genitals or anus. Herpes has two variants:
- HSV-1 (oral herpes) causes fever, blisters and cold sores around the lips.
- HSV-2 (genital herpes) causes sores around the anus and genitals.
Genital warts
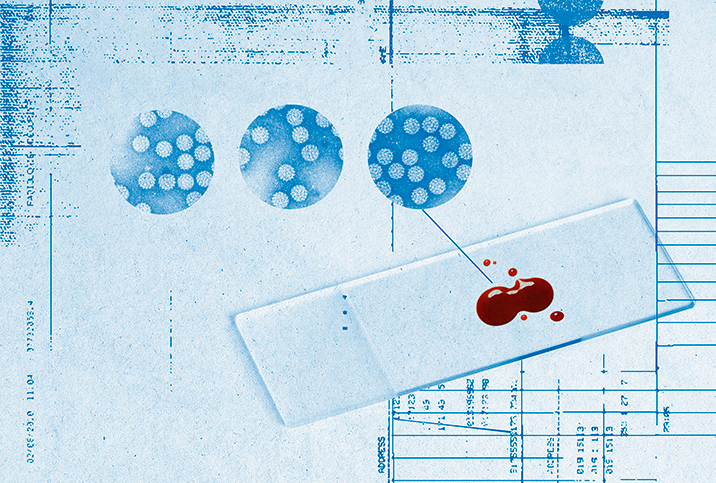
Genital warts are growths caused by the human papillomavirus (HPV), which is transmitted by skin-to-skin contact, usually in the areas of the genitals not covered by condoms. HPV can be transmitted into the oral and throat cavities through mucous membranes, too. The disease has been associated with many kinds of cancer, including cervical and throat cancers.
Symptoms of genital warts include:
- Painless lumps and growths around the penis, vagina or anus
- Itching and bleeding from the penis, vagina or anus
- Abnormal urine flow in men if the genital warts are present in the urethra
- Your partner develops genital warts, even if you don't have symptoms yourself
Swarup added that HPV usually doesn't have any symptoms, so a person can carry the disease without having genital warts. HPV has many strains, some of which manifest in warts, others which increase cancer risk if untreated.
Chlamydia
Chlamydia is a common sexual infection that affects both men and women. Some people never experience any symptoms, however, the signs that do show can include:
- Painful urination
- Unusual discharge from the penis, vagina or anus
- Pain in the stomach and bleeding after sex and between periods
- Pain, tenderness and swelling in the testicles
Gonorrhea
Like chlamydia, gonorrhea does not always present symptoms. The main symptoms may include:
- A green or yellow discharge from the penis or vagina
- Painful urination
- Bleeding between periods
When discussing signs and symptoms of STDs, it's vital to include HIV (human immunodeficiency virus). A major sign of HIV is flu-like symptoms within two to four weeks of getting the virus, according to Swarup. However, some people may not feel sick until the infection becomes more serious.
Misconceptions about STDs
STDs are very common and easily spread when condoms or other barrier methods are not used, Swarup said. They can occur if safer sex methods fail, so it's critical to learn how to use your barriers correctly.
"Some STDs can be life-threatening to yourself and any sexual partners," Swarup added. "HPV causes 99 percent of cervical cancers; HIV untreated can be fatal; and syphilis long term can have a negative effect on many organ systems."
The damage syphilis causes can be irreversible if not identified and treated in time.
Latex condoms can reduce the chance of passing on STDs such as chlamydia and gonorrhea, Murphy said.
"However, genital ulcer diseases and HPV are not protected," she noted. "This is because these STDs occur in areas not covered by condoms. Luckily, consistent use of certified latex condoms can reduce your chance of contracting genital herpes, syphilis and other ulcer diseases if the infected area is fully covered and protected."
Condom use can also reduce the risk of HPV or HPV-associated diseases such as cervical cancer.
"Theoretically, the condom's effectiveness depends on the sore, ulcer or infection location," Murphy said, adding that the integrity of the affected skin or mucosa also plays a role. "Condoms will only protect against transmission if it is completely covered."
A condom can slip down the penis or tear during sex, rendering it less effective. Therefore, a condom can't be relied on to prevent ulcers and warts as effectively as it would prevent other types of STDs.
How to improve a condom's efficiency
Murphy provided seven tips to ensure your condom is as effective as it can be against STDs:
- Use only condoms that fit: A correctly sized condom minimizes your chances of acquiring an STD. If the condom is too big, it can slip off. If the condom is too small or tight, it can tear or break during sex.
- Store your condoms correctly: Store condoms in a dry and cool place, such as a bedside drawer or cardboard box. Do not store condoms in a wallet or anywhere that causes friction, as this may compromise the condom and render it useless.
- Check your condom is up to date: If the condom is out of date, it can break down and become less effective, increasing the risk of STD transmission.
- Use only your hands to open a condom: You may tear, break or otherwise damage the condom if you use your teeth or scissors to open a condom package. Use only your fingers.
- Put the condom on before you have sex: You must put a condom on before your penis comes into contact with the vagina or anus to protect yourself from STDs. You can transmit STDs through grinding, scissoring, outercourse and intercourse.
- Make sure your condom is the right way around: Be sure to put the condom on correctly the first time. If you start to roll the condom down your penis and realize it is inside out, don't flip it over; throw it away and get a new one. There should be a reservoir at the top of the condom where the ejaculate goes when you orgasm. If you don't leave a space, ejaculation may cause the condom to tear.
- Always throw your condom away safely: Once you have ejaculated or otherwise finished having sex, prevent spillage by holding your condom when you remove your penis from your partner. You can run water into the condom to ensure it hasn't broken during sex; if water does not leak out, the condom has done its job. Then tie the condom to stop fluid from spilling out, wrap it in tissue and put it in a bin. Remember, condoms are not flushable.
Reducing the risk of STD transmission
While condom use may be associated with a lower risk of cancer, condoms should not be the only preventive measure you take with your partner, Murphy advised.
"Women should go for regular Pap smears to detect or prevent cervical cancer," she said. "In addition, people should also get the HPV vaccination if eligible and use condoms."
"As well as practicing safe sex, it is important to get tested frequently and share your history with your partner and your healthcare provider," Swarup said.
Murphy suggested asking your sexual partner about their STD status while you share your results.
“This stops you from coming across like you are making accusations and makes the decision to disclose your STD status a shared one,” she explained.
Murphy advised asking your partner in the following ways:
- Before we have sex, you should know I was last tested (give date), and I've had (disclose number) partners since. When were you last tested?
- Would you like to be tested together before having sex?
You should be honest about how many other partners you're seeing, how frequently and other information you feel may be relevant to your sexual health.
If you are experiencing any STD symptoms as described above or are sexually active, get tested—maybe on a regular basis, depending on your doctor's opinion and discretion.
"People should get regular tests for all STDs, especially if they intend to sleep with new people," Murphy said. "This involves getting tested for oral and anal STDs if you plan to have anal or oral sex. Typically, all sexually active people should get tested annually."
Even in monogamous relationships, it's beneficial to get tested during your checkups with your primary care physician.