Deep Brain Stimulation Surgery Can Help OCD...Sometimes
When Haley was 7, she began treatment for obsessive-compulsive disorder (OCD). She's been through extensive exposure and response prevention therapy (ERP) and two rounds of radically open dialectical behavior therapy (RO DBT). She's also been on many medications with augmentation and completed transcranial magnetic stimulation (TMS).
Now an adult, her obsessive-compulsive disorder has become worse over the past six years.
"OCD has impaired my ability to go outside, cook or even enter a kitchen, communicate, write/read, do laundry, throw things away, go shopping, drive, sleep in my own room, and more," she wrote on Instagram.
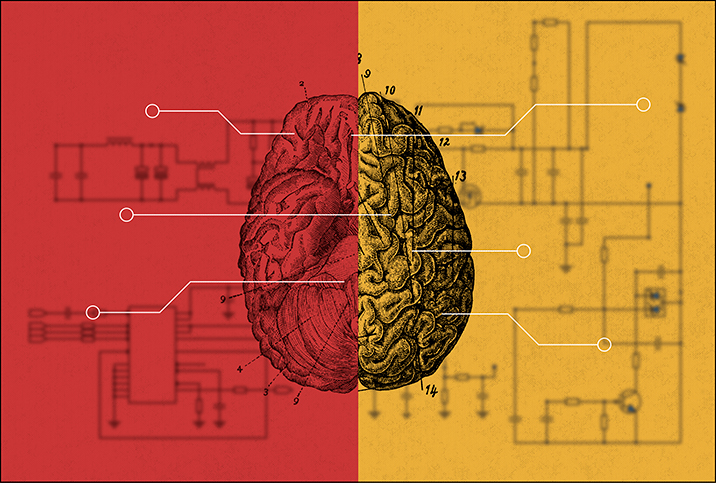
Brain scans can detect which part of your brain is causing your symptoms, and electrodes are implanted to send electrical signals to mitigate the symptoms.
Haley's ongoing experience with debilitating and refractory OCD led to her being approved last year for deep brain stimulation (DBS) surgery. In May 2021, she had her first of three surgeries to place a DBS device in her brain.
"Deep brain stimulation is a surgical technique which has been around since the late 1970s in which a small electrode, less than 2 millimeters in width, is threaded via 'burr holes'—holes about the size of a quarter in the skull—to a specific part of the brain to change the electrical circuitry," explained Ankur A. Butala, M.D., assistant professor of neurology, psychiatry and behavioral sciences at Johns Hopkins University School of Medicine.
Electrical impulses can help
Since its creation, DBS has largely replaced lesion-based procedures. The first surgeries were for tremors—essential tremor or Parkinson's disease, for example—but DBS has been beneficial to patients with a number of different illnesses.
"Over the last 10 to 15 years, earlier work in Tourette syndrome—a disorder of the nervous system that presents as unwanted sounds or repetitive movements—and depression led to expanding study into other disorders, such as obsessive-compulsive disorders or even schizophrenia. We have performed DBS for a person with schizophrenia here," Butala explained.
DBS uses electrical impulses to treat OCD and is effective for about 60 percent of patients, according to the Mount Sinai Center for Neuromodulation in New York City. Brain scans can detect which part of your brain is causing your symptoms, and electrodes are implanted to send electrical signals to mitigate the symptoms. Candidates are eligible only if they have severe obsessive-compulsive disorder and have tried—and failed—other forms of treatment, such as medications and therapy, like Haley did.
After Haley's first DBS surgery, she underwent two more surgeries to place a second electrode in her brain and a neurostimulator in her chest.
"We implant a neurostimulator, a small device similar to a pacemaker, that delivers mild electrical signals. We put the device near your collarbone. Then we connect the electrodes, which carry the electrical current to the neurostimulator," the Mount Sinai website stated.
Naturally, these surgeries have been anxiety-inducing for Haley, even if they are meant to help mitigate her obsessive-compulsive disorder symptoms, a situation that creates a vicious cycle.
"My OCD has completely latched on to my anxiety," Haley wrote on Instagram. "For example, to ensure that this surgery goes as smoothly as the last two, I am having thoughts that I need to wear the exact same outfit I wore to the hospital for the first two surgeries and do the exact same activities the day before surgery."
Controlling stimulation levels
The next step after surgery is turning on the devices so they can communicate to each other and to the brain.
"I am the 3rd or 4th person in the world to have a device that can record brain waves so he turned that feature on," Haley wrote on Instagram. "[My doctor] has already seen an abnormality in my brain wave that he believes could be contributing to my symptoms."
After her doctors turned on the device, they programmed the stimulation levels based on how her anxiety, depression and energy felt at each setting.
Today, Haley is hopeful about her DBS journey. She continues to check in with her doctors to adjust her stimulation levels and settings on her DBS device. She continues to do ERP therapy and take medication. Haley also recently started college.
"I'm feeling optimistic that this semester will be different with DBS and that I can make some real progress on my OCD," she wrote. "It's my job to do the opposite of what my OCD wants me to do. It's a struggle but I have to prevail so that I can live my best life."




















