Stopping Estrogen-Containing Birth Control Cuts Blood Clot Risk
Key Points
- The risk of developing a blood clot from combined hormonal birth control methods is slim, especially compared to the chances of developing a blood clot while pregnant or postpartum.
- People taking estrogen-containing contraceptives are about three times more likely to get clots compared to those who don’t.
- A new study suggests a person’s likelihood of developing a clot decreases dramatically within weeks of stopping hormonal birth control.
Hormonal contraceptives are some of the most popular and effective ways to prevent pregnancy and manage irregular, painful or heavy periods. They're also safe but not entirely risk-free.
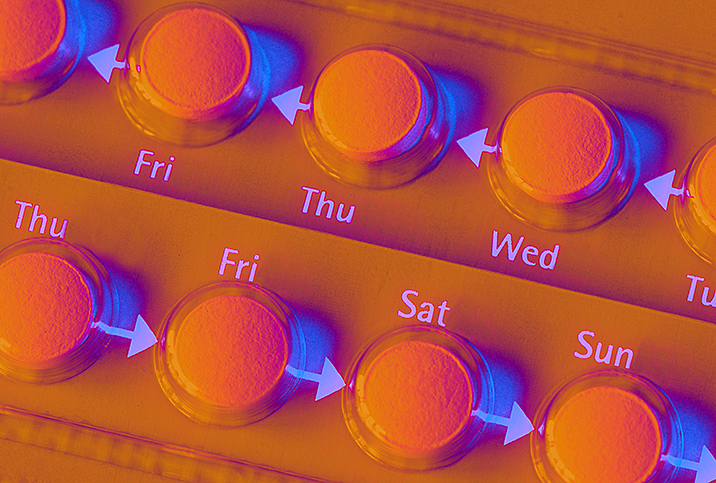
Combined hormonal birth control methods, such as the birth control patch and pill, can increase the chances of a blood clot threefold. A new study suggests that clotting risk disappears within a few weeks of stopping use.
Can birth control cause blood clots?
Clotting is necessary for wound healing, but abnormal clots can block blood vessels and restrict blood flow to the heart, according to the American Society of Hematology (ASH).
The most common example is deep vein thrombosis (DVT), which usually occurs in the legs.
Unaddressed, DVT can lead to a clot in the lung, known as a pulmonary embolism (PE), which can be fatal.
People who take certain types of birth control are slightly more likely to develop DVT or PE than those who don't, according to the U.S. Food and Drug Administration (FDA).
"The risk is most closely associated with combined hormonal contraceptives, which come in the form of pills, vaginal rings and skin patches," said Kate Arnold, M.D., OB-GYN, the co-founder of FemInnovation in Washington, D.C.
This type of birth control contains estrogen and progestin rather than progestin alone.
Additionally, some studies suggest hormonal contraceptives that contain drospirenone, a type of progestin, may carry a higher blood clot risk compared to those containing levonorgestrel or other forms of the hormone, according to the FDA.
Other studies have found no additional risk, however.
Drospirenone is used in combined hormonal contraceptives, including products marketed by the brand names Beyaz, Ocella, Safyral, Yasmin, Yaz and Zarah.
The administration method could also make a difference, according to the National Women's Health Network. Some evidence suggests vaginal rings and patches, which provide a continuous dose of hormones, are more likely to cause blood clots than the pill.
"The chances of developing a clot from any form of birth control are slim," said Adi Davidov, M.D., the associate chair of obstetrics and gynecology at Northwell Staten Island University Hospital in New York City.
Between 1 and 5 women in 10,000 who aren't pregnant and don't use birth control pills will develop a problematic blood clot in a given year, per the FDA. Comparatively, between 3 and 9 people in 10,000 who use combined pills will get one.
The chances are significantly higher for pregnant people and those in the 12-week postpartum period. In these populations in a given year, between 5 and 20 pregnant women in 10,000 run the risk of developing a blood clot. For those in the 12-week postpartum period, between 40 and 65 out of 10,000 will develop an abnormal clot.
Intrauterine devices (IUDs) and progestin-only injections, implants, and pills that don't contain estrogen or drospirenone aren't thought to affect clot risk.
Why does birth control cause blood clots?
Estrogen affects coagulation factors in the blood. Drospirenone potentially does, too.
"Also known as clotting factors, these proteins make the blood clot more easily," said Nandita Palshetkar, M.D., OB-GYN, a fertility specialist in Mumbai affiliated with ClinicSpots. "Think of it like making the blood a bit 'stickier.' This increased stickiness helps prevent bleeding during childbirth.
"But it can also increase the risk of forming clots when not pregnant, especially in the veins of the legs, which can potentially travel to the lungs."
How quickly can birth control cause blood clots?
"The risk of blood clots increases soon after a person starts using combined hormonal birth control," Arnold said.
It remains highest for the first several months of use.
"The risk is also elevated each time a woman starts taking contraceptives after a break," Palshektar said. "It's not that clots will necessarily form immediately, but the risk is there as long as the contraceptives are being used."
Recommended
- Your Sex and Hormones Impact Your Risk for Deep Vein Thrombosis: A woman's hormones increase her risk for DVT at certain times in her life.
- Selecting the Birth Control That's Right for You: When it comes to birth control, choose the type of birth control that's best suited to your lifestyle.
- Birth Control: Myths & Misconceptions: Don’t let misinformation keep you from finding your best method of contraception.
What can increase your risk of getting a blood clot when taking birth control pills?
Deep vein thrombosis and pulmonary embolism most often occur in people with specific health problems that make them more vulnerable to clots. These health problems include:
- Reduced blood flow
- A genetic predisposition to irregular clotting
- A recent injury
Doctors typically advise women with such conditions to use a nonhormonal or progestin-only contraceptive unless they're taking anticoagulant medication, according to the National Blood Clot Alliance.
Reduced blood flow
"When blood cannot move freely through the body, clots are more likely to occur," Arnold said.
Underlying health conditions—atherosclerosis, high blood pressure, diabetes, varicose veins, obesity, peripheral artery disease—can adversely affect circulation, according to Cleveland Clinic.
Age may also decrease blood flow, according to the National Library of Medicine.
"Being immobile for long periods, such as on a long-distance flight or when bedridden, can also raise DVT risk by allowing blood to accumulate in the legs," Palshetkar said.
Unusual clotting
"Some conditions—such as the factor V Leiden genetic mutation and antiphospholipid syndrome—can make a person's blood clot more easily," Davidov said.
People with a family or personal history of clots are also more likely to develop them.
Additionally, having cancer may increase a person's risk, according to Memorial Sloan Kettering Cancer Center. Genetic changes that cause cancer can increase clotting factors, as can many chemotherapy drugs.
Injury
Trauma, especially to the legs, can raise the likelihood of a clot for a couple of reasons. For one, it may damage the vein's inner lining, according to the University of Connecticut. This can occur from serious injuries, surgery, inflammation or immune responses.
Additionally, injuries may increase clot risk if they restrict mobility; for example, if someone's in a cast or bedridden.
What does the new study indicate about blood clots after stopping birth control?
For the new study, researchers evaluated blood samples from 66 women who took hormonal contraceptives such as pills, skin patches or vaginal rings. Participants provided samples six times while taking hormonal contraceptives and within three months of quitting. Researchers compared these samples to those of 28 women who didn't use hormonal contraception.
The researchers found that within two weeks of stopping hormonal birth control, levels of clotting factors in participants' blood fell by 80 percent. Within four weeks, levels declined by 85 percent. By week 12, levels were similar to those in the control group.
"These findings can help to inform discussions around whether combined hormonal contraceptives are right for the patient, as well as patient-surgeon discussion of whether the benefit of stopping for a short time actually exceeds the risks," said Marc Blondon, M.D., a vascular medicine expert at the University Hospitals of Geneva, Switzerland, and the study's corresponding author, in a press release.
"It's very important to talk about the benefits of contraception because it's crucial to avoid unwanted pregnancy and for women to have the choice of a planned pregnancy," he added.
The findings were published in Blood, a journal of the ASH.
"The study is encouraging and should help patients feel empowered to stop their hormonal birth control and opt for barrier or progesterone-only methods if they find they have other risk factors for developing blood clots," Arnold said.
Should You Be Sweating to Help Your Fertility or Menstrual Cycle?: Some people believe infrared saunas can help conditions from painful periods to fertility.
What should women know about the risk of blood clots while using birth control?
Deciding what type of birth control to take is a highly personal process, and assessing blood clot risk is one of many essential factors to consider.
"For many people, the benefits of combined hormonal birth control methods outweigh the risks," Blondon said. "Aside from reducing the chances of an unplanned pregnancy, estrogen-containing contraceptives have been found to alleviate pelvic pain disorders and reduce the risk of anemia and endometrial and ovarian cancers."
Circumstances do exist in which people may want to stop or avoid combined hormonal contraceptives, Arnold added. A big one: if they develop or discover an underlying health condition that potentially increases their chances of abnormal clotting.
Doctors may also suggest stopping hormonal birth control ahead of elective surgery or while recovering from a clot, to reduce the risk.
"Although DVT and PE can be asymptomatic, knowing the signs of these conditions is imperative," Palshektar said.
She suggested seeking medical care immediately if you experience any of the following symptoms:
- Chest pain
- Coughing up blood
- Fainting
- Lightheadedness or dizziness
- Pain or tenderness in a leg or arm
- Rapid pulse
- Shortness of breath
- Unexplained swelling
The bottom line
Blood clots are uncommon and usually occur in women who are pregnant and those with health problems that affect blood circulation or coagulation. Talk to your doctor before starting or stopping any kind of medication, including combined hormonal birth control methods, to ensure it's safe to do so.
"It's really important for everyone to understand that the increased risk of blood clots with estrogen-containing birth control is still less than half the risk someone who is pregnant faces," Arnold said. "With that said, taking estrogen-containing birth control is a personal choice that should always take into account a person's health factors and their wishes."