Do Crohn's and Colitis Cause Oral and Sexual Health Problems?

Inflammatory bowel disease (IBD) includes conditions such as Crohn's disease and ulcerative colitis. These two forms of IBD can have varying and widespread consequences on an individual's health and quality of life. According to the Centers for Disease Control and Prevention (CDC), about 3 million Americans have been diagnosed with IBD, which is almost 1 in 100 people.
It's important to understand the potential effects of inflammatory bowel disease on oral and sexual health. What are the links between IBD and sexual health based on the current literature? How can people who suffer from IBD make informed decisions?
'If you're suffering from painful changes within your mouth you should address those concerns immediately.'
Living with inflammatory bowel disease can be challenging, but there are strategies that can help you avoid some of the risks associated with this condition and improve your sexual health.
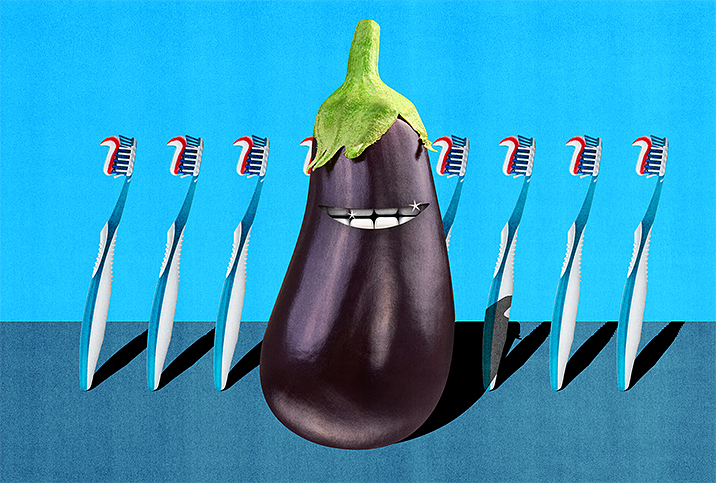
How is oral health involved with IBD?
"Inflammatory bowel disease is an umbrella term used to describe a range of chronic and long-term conditions that involves inflammation in the gastrointestinal tract," said Samrat Jankar, M.B.B.S., M.S., a gastroenterologist, colorectal surgeon and laparoscopic surgeon in Pune, India. "People living with IBD are at greater risk of developing oral health issues, due to both the condition itself and certain treatments they may be receiving for their condition."
According to researchers, people with inflammatory bowel disease are more likely to experience various adverse oral manifestations. These include:
- Aphthous ulcers. Commonly known as canker sores, these are small, shallow, painful lesions that can develop on the soft tissues in the mouth or at the base of the gums.
- Cobblestoning. This refers to a particular appearance of the oral mucosa (the lining of the mouth) where it takes on a bumpy or cobblestone-like texture. This is a specific manifestation often associated with Crohn's disease.
- Gingivitis. This is a typical form of gum disease that causes gum inflammation. It's often the result of poor oral hygiene and left untreated can lead to more serious gum disease such as periodontitis and tooth loss. Researchers note people with IBD are at a significantly higher risk of periodontitis.
- Lymphadenopathy. This refers to the condition of having enlarged lymph nodes, which can occur in various parts of the body, including the neck and jaw area near the mouth.
- Oral soft-tissue lesions. Abnormalities can appear on the soft tissues of the mouth, such as the tongue, cheeks and gums. They vary in appearance and may include sores, lumps or areas of discoloration.
- Pyostomatitis. This is a severe form of stomatitis, an inflammation of the mouth and lips, which is characterized by the presence of pus-filled sores.
"Oral bacteria can travel throughout your body and even to the gut through the saliva. There are some bacteria that get destroyed by the stomach's acid," said Fatima Khan, D.M.D., a doctor of dental medicine at Altus Dental in Baytown, Texas, a general dentistry practice. "However, others are acid-resistant, such as Porphyromonas gingivalis [aka P. gingivalis]. Porphyromonas gingivalis is linked to gut microbiome imbalance or dysbiosis. In the oral cavity, this bacteria is linked to periodontal disease also known as gum disease."
Additionally, those strains are able to pass through the stomach to the intestines and colon. There, they can cause inflammation and dysbiosis of the gut, Khan added. Such an imbalance can cause inflammatory bowel disease and obesity.
"Crohn's and colitis involve the entire gastrointestinal system from the mouth to the anus and often affect oral health," said Inna Melamed, Pharm.D., a functional medicine practitioner and gut and hormones expert in Marlboro, New Jersey, and the author of "Crohn's and Colitis Fix" and "Digestive Reset." "Since the immune system response isn't properly regulated and mostly lowered, it becomes easier for the gums to get inflamed."
How IBD affects oral health
The relationship between inflammatory bowel disease and oral health is complex and multifaceted. According to experts, oral issues may arise from the direct inflammatory nature of IBD itself, and this is more likely with Crohn's than colitis. However, both forms of IBD can lead to indirect effects on oral health, such as nutrient deficiencies and the side effects of medications.
Nutrient deficiencies
This is caused by the poor absorption of essential vitamins and minerals. Iron deficiency, a common occurrence in IBD patients, can lead to a condition known as angular cheilitis, characterized by sore and red corners of the mouth.
Side effects of medications
Drug classes used to treat IBD may have toxic effects on oral tissue. Certain IBD medications can lead to oral health issues, such as dry mouth or increased susceptibility to oral infections.
Neglecting oral health can significantly impact one's sexual health in general. But anyone who suffers from inflammatory bowel disease needs to be mindful of their oral health, which becomes even more crucial due to the increased risk of developing numerous oral health issues.
IBD patients are at an increased risk of periodontal disease, which has been linked to erectile dysfunction (ED) in men. Additionally, poor oral health may impact the balance of the oral microbiota, which in turn could influence the health and function of multiple human systemic diseases.
While more studies are needed to fully understand many of these links, there is no doubt that poor oral health has far-reaching implications for multiple systems, including the reproductive system.
"IBD is still considered an 'embarrassing' disease since diarrhea can interfere with sex life, intimacy and relationships," Melamed said. "And bad breath can be something that affects relationships and work. IBD patients with inflamed gums are even afraid to smile, and that may become something that creates loneliness, the new epidemic of our time."
Maintaining good oral hygiene is important
Oral hygiene is vital to a person's well-being. Consider going for regular dental checkups, brushing and flossing daily, and maintaining a healthy and balanced diet. Use a soft toothbrush for gentle cleaning and to reduce any discomfort in the mouth. Alcohol and tobacco can exacerbate oral health issues. So can sugary and acidic food and drinks. People need to take this into account when considering these kinds of lifestyle choices.
Open communication with your partner is essential. Discuss your inflammatory bowel disease and how it affects you, because opening up can help alleviate some emotional and psychological stress. If you're experiencing sexual difficulties, consider seeking help from a healthcare provider or a certified sex therapist.
Regular exercise can help boost your energy levels and improve your body image, thereby improving sexual health. Additionally, your healthcare provider may recommend dietary supplements if you suffer from any nutrient deficiencies due to IBD.
Ultimately, Crohn's and colitis can impact oral and sexual health, but these problems can be managed with proactive healthcare and lifestyle modifications. Be open to guidance and support as you navigate these challenges and take back control of your sexual well-being.
Discussing any concerns you have about your oral or sexual health with your healthcare provider is one of the most important steps to ensuring proper care and avoiding conditions such as cheilitis (inflammation of the lips).
"Cheilitis can be seen with Crohn's disease, and less commonly, ulcerative colitis," said Jacquelyn Charbel, D.O., a colorectal surgeon at Michigan State University Healthcare in East Lansing. "When the inflammation or pain is located at the corners where the upper and lower lips meet, it is known as angular cheilitis."
Skin redness and scaling may be present near the lips, she added. In addition, glossitis—inflammation of the tongue—is sometimes seen.
"Ulcerations within the mouth and stomatitis (inflammation of the oral mucosa) are present in nearly one-third of patients with Crohn's disease," Charbel said. "Rarely, pyostomatitis vegetans may be present, which is a pustular sore within the mouth. When present on the skin surrounding the mouth, it is known as pyodermatitis vegetans."
These problems are more common in men, and oral examinations of such symptoms can be the catalyst that leads to IBD diagnosis, Charbel said. If you're suffering from painful changes within your mouth you should address those concerns immediately.
"Something as seemingly small as new-onset dry mouth or halitosis (bad breath) may be a signal of an underlying autoimmune disorder," Charbel said. "These issues can lead to tooth decay and gum infection. Make sure to keep up with your dental checkups at least every six months."