How to Get Properly Diagnosed and Treated for IBD

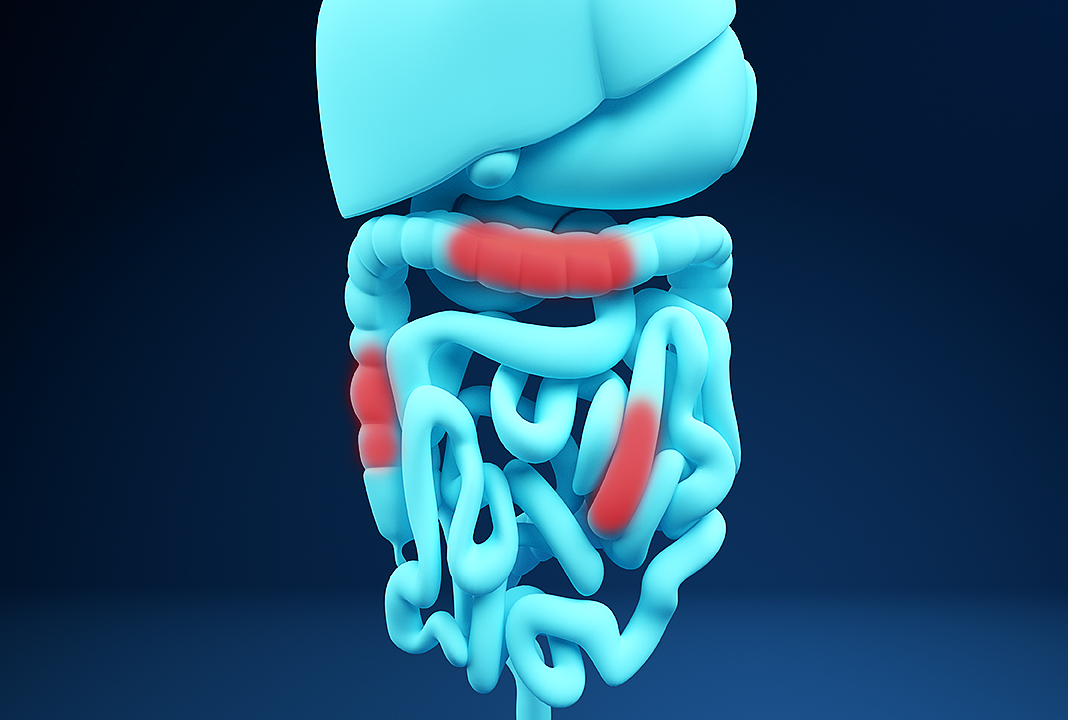
Inflammatory bowel disease (IBD) is a lifelong condition. The disease cannot be cured and treatment strategies typically revolve around managing symptoms and keeping inflammation under control. This principle applies to both Crohn's disease and ulcerative colitis, the two diseases of the intestinal tract that fall under the umbrella of IBD.
IBD is generally diagnosed in youth. Researchers claim about 10 percent of patients diagnosed with Crohn's disease are younger than the age of 17. However, inflammatory bowel disease can develop later in life, as research indicates up to 15 percent of patients are diagnosed past the age of 60.
Regardless of whether a person is diagnosed with Crohn's disease or ulcerative colitis, structuring a treatment plan depends on the severity of the case and often varies between individuals. Inflammatory bowel disease usually gets diagnosed after a patient experiences their first or second "flare up," a spike in gastrointestinal inflammation accompanied by pain and a variety of other symptoms.
Aside from your physical health, inflammatory bowel disease can lead to problems involving your sexual health, too. Although there's no reason IBD patients cannot be intimate, the course of the disease, medication and possible surgical solutions necessary for some people—as well as the general symptoms—can get in the way of creating an ideal atmosphere for sexual activity.
Certain disease symptoms, medications and surgeries can also impact libido and potentially cause erectile dysfunction (ED) in men.
There is not a lot of recent research on this condition, but it's estimated by the Crohn's & Colitis Foundation that about 40 percent of IBD patients report the disease has prevented them from forming intimate relationships. Close to 70 percent of IBD patients claim to have body image problems.
Sexual dysfunction is reported by 52 percent of women and 20 percent of men with inflammatory bowel disease.
Diagnosis comes first
Your gastroenterologist's first goal is to diagnose the type of inflammatory bowel disease that has developed, and the process may involve conducting a colonoscopy, upper endoscopy, MRI (magnetic resonance imaging) or CT (computed tomography) scan in order to establish whether the patient has Crohn's disease or ulcerative colitis.
In some cases, your diagnosis may not be obvious, and your doctor will probably diagnose you with indeterminate colitis until further investigation uncovers the root cause of your symptoms.
Medications involved in treating and managing both forms of inflammatory bowel disease are generally the same, according to a research study published in 2020, and are mainly composed of anti-inflammatory drugs and immunomodulators. However, keep in mind that the efficacy of these medicines and the choice of treatments may vary depending on the specific condition or individual.
"It isn't possible to cure IBD, so the aim of the treatments—that will most likely consist of certain drugs—is to reduce inflammation that triggers symptoms and to keep patients as long as possible in remission," said Jelena Vulevic, Ph.D., a gut microbiologist in the United Kingdom with 20 years of experience and the CEO of veMico, a research and development company for biological therapies. "The choice of exact treatment depends on the site and severity of the disease as well as a patient's overall health and response to treatment."
'The course of the disease, medication and possible surgical solutions necessary for some people—as well as the general symptoms—can get in the way of creating an ideal atmosphere for sexual activity.'
As mentioned earlier, IBD is typically diagnosed after a patient experiences their first flare-up, which is the point when inflammation peaks. The accompanying treatment plan should aim to induce remission and drop inflammation down to baseline/tolerable levels.
Each subsequent spike or inflammatory flare-up during the course of a patient's life will slightly raise the baseline, gradually wearing away at the gastrointestinal tract with time. The severity of inflammatory bowel disease typically correlates with how long a sufferer has had the disease.
It is helpful to think of inflammatory bowel disease as a relapsing-remitting condition, whereas the goal is to induce a prolonged state of remission and prevent relapse or flare-ups. Unfortunately, this process isn't cheap. Research indicates treatment costs are rising and often underestimated, with the average cost of care being about $22,987 per year in the United States.
Conventional treatment
There are three main classes of medication for inflammatory bowel disease, and treatment may involve a combination of different medications depending on each case.
Anti-inflammatory drugs
A patient suffering from their first flare-up will be prescribed anti-inflammatory drugs in order to start inducing remission and reducing inflammation. There are two main categories:
- Aminosalicylates. The most common form of this medication is known as 5-aminosalicylic acid (5-ASA). According to the European Crohn's and Colitis Organization (ECCO), 5-aminosalicylic acid is generally safe, reduces the chances of relapse and significantly mitigates the risk of developing colorectal cancer. In general, this drug is reserved for mild to moderate cases and is used to induce remission upon flare-up; it may be recommended for long-term maintenance purposes.
- Corticosteroids. These steroids are typically reserved for cases where the initial 5-ASA treatment plan proves to be ineffective. Experts recommend starting with corticosteroid medications such as prednisone and budesonide. Treatment should commence if the patient is not responding to aminosalicylates after two to four weeks. Steroids are highly effective at inducing remission but are only recommended on a short-term basis because they are associated with significant side effects. Corticosteroids should not be used for maintenance, but only for inducing remission.
Immunomodulators
It's generally accepted that inflammatory bowel disease is linked to an inappropriate immune response. As the name suggests, immunomodulators are medications used to modulate the immune system to induce or maintain remission. According to a review paper published in 2016, 60 percent of patients with IBD receive thiopurines, which are a class of immunomodulatory medication. Thiopurines are an effective maintenance therapy for Crohn's disease and ulcerative colitis, and there are two primary types:
- Azathioprine (AZA)
- Mercaptopurine (MP)
Another widely used immunomodulatory medication is methotrexate (MTX), but this is only recommended for relapse prevention in patients with Crohn's disease.
As stated in the 2016 review, up to 33 percent of patients who take thiopurines experience adverse side effects, forcing them to discontinue treatment. As mentioned earlier, immunomodulators affect the immune response and can impact the number of white blood cells in the body, leaving patients at a higher risk of infection. Other potential side effects include gastric intolerance, pancreatitis and hepatotoxicity (liver damage). This is further corroborated by a large-scale study published in 2009 in the Lancet linking thiopurines with an increased risk of developing various lymphoproliferative disorders.
Biological medicines
This is the latest innovation in the treatment of inflammatory bowel disease. Traditionally, biological agents and therapies were only considered upon failure of anti-inflammatory drugs and immunomodulatory medications. However, more practitioners have begun recommending biologics early on in the treatment process.
According to experts in an article published in 2019 in Inflammatory Bowel Diseases journal, early adoption of a group of biologics known as anti-tumor necrosis factors (anti-TNFs) could significantly alter disease progression in the long term, reducing the need for surgery by up to 40 percent. These medications include:
- Adalimumab
- Certolizumab
- Infliximab
According to Crohn's and Colitis UK, adalimumab and infliximab have been shown to treat fistulizing Crohn's disease, which is considered a severe case.
Alternative biological agents used for IBD treatment include the anti-integrin vedolizumab and the anti-IL-12/23 ustekinumab. However, these are generally reserved for cases where the anti-TNF medications are ineffective or have stopped working.
'Prebiotic fiber (found in garlic, bananas, flaxseed and asparagus), which feeds the good bacteria in the gut to produce health-promoting metabolites such as butyrate, can be useful in the treatment of ulcerative colitis and Crohn's disease.'
Aside from certain drugs and biological medicines, there are other treatment options as well.
"Other options include antidiarrheal medications, pain-reducing antispasmodics, vitamins, herbs and supplements," said Inna Melamed, Pharm.D., a functional medicine practitioner and gut and hormones expert in New Jersey, and the bestselling author of "Crohn's and Colitis Fix" and "Digestive Reset." "Some holistic and functional medicine options also include good nutritional protein support as well as anti-inflammatory supplement support."
Lifestyle modifications
When diagnosed with inflammatory bowel disease, your doctor, nutritional therapist or dietitian may recommend various lifestyle changes in order to prevent further flare-ups in the future.
"From a nutrition point of view, to prevent IBD or any gut inflammation, it is recommended to consume a high-fiber diet," said Amani Kaite, a London-based nutritional therapist specializing in gut health. "Government guidelines say our dietary fiber intake should be at least 30 [grams] a day. Fiber acts like a broom that sweeps the intestines of buildup and can reduce the risk for colon cancer."
She added that prebiotic fiber (found in garlic, bananas, flaxseed and asparagus), which feeds the good bacteria in the gut to produce health-promoting metabolites such as butyrate, can be useful in the treatment of ulcerative colitis and Crohn's disease. Stress is known to cause low-grade intestinal inflammation, and people with IBD are very often living in sympathetic overdrive, in a "fight-or-flight" state. Therefore, calming activities such as yoga, breathwork and meditation can help reduce stress and build happiness.
'Many have a very significant drop in libido due to adrenal hormone production imbalance. Many are too fatigued to have a sexual desire. And constantly being in pain doesn't help, either.'
A nutrition expert can help create an anti-inflammatory diet plan based on the patient's preferences and nutritional needs, Kaite said. She also advised talking to a nutrition expert—ideally, someone who specializes in gut health—and not trying to figure it out on your own, as self-prescribed dietary restrictions may lead to severe nutrient deficiencies.
Don't hesitate to talk to your healthcare professional if your nutrient absorption is reduced.
"If nutrient absorption is reduced due to frequent episodes of diarrhea, for example, or the person starts losing weight, then it's very important to talk to your healthcare professional and to include supplementation of vitamins and minerals that become depleted," Vulevic explained. "It's not a good idea in this case especially to try and self-medicate. The use of certain supplements to strengthen gut health and immunity is a very good idea in IBD. These can also sometimes help with certain symptoms as well as the efficacy of the medication. There are very many on the market."
Additional support through supplementation is recommended. However, keep in mind that some drugs can interfere with nutrient absorption, which is why IBD patients shouldn't self-medicate and instead should talk to a professional beforehand.
"Nutritional supplements are strongly recommended for IBD sufferers as they may need extra help to reduce inflammation, support the immune system and prevent nutrient deficiencies," Kaite advised. "Targeted supplements include vitamin D, vitamin B12 and zinc, gut-healing herbs such as chamomile and slippery elm and probiotics. Some drugs don't work well with certain vitamins or can interfere with the absorption of certain vitamins, so IBD sufferers should always talk to their healthcare practitioner before supplementing."
How IBD affects sexual health
According to Kaite, most people with inflammatory bowel disease are capable of being intimate. However, the stress from having the disease, taking the medications or having surgery can sometimes affect sexual drive.
"IBD has a heavy effect on sexual health," Melamed explained. "Many people suffering from diarrhea are very embarrassed to be in sexual relations. Many have a very significant drop in libido due to adrenal hormone production imbalance. Many are too fatigued to have a sexual desire. And constantly being in pain doesn't help, either."
Orli Rhodes, a dietitian at King Edward VII's Hospital in London, added that its psychological impact can sometimes make people feel uncomfortable.
"Inflammatory bowel disease has no direct impact on sexual function, however, the psychological impact can sometimes cause individuals to feel uncomfortable with their body image," she added. "If patients are suffering for something, [they] should be as open as possible and ask for help.
"Side effects of treatment may impact a patient's interest in sex and intimacy or [cause] complications such as erectile dysfunction in men," Rhodes continued. "IBD can be very disruptive to those affected and limit their interest in sex; having to work around symptoms like diarrhea and extreme tiredness may impact their sex drive. But with symptoms managed effectively, there's no reason a patient can't go on to enjoy sex and intimate relationships."
IBD and the immune system
"IBD is the result of the immunological imbalance as well as an inappropriate GI microbiota makeup, which is also significantly related to the immune function," Vulevic explained. "Furthermore, disease progression, symptom duration and severity, coupled with the use of nearly all medications, cause further damage and/or the suppression to the immune system function. Thus, the impact on the immune system is significant in all cases. For this reason, it's very important to keep the remission state for as long as possible, to adopt best practices when it comes to a healthy lifestyle and diet, and to take good supplements that aim to strengthen gut health and, therefore, immune system function."
Melamed added that IBD is directly related to immune system health. The reaction of the system to stress, environmental factors, pathogens and so on isn't adequate, and this creates an unexpected response. Therefore, she said immunocompromised people on drug therapy for IBD should be very careful around flu season and around hospitals, and consider basic protective techniques, hygiene and taking natural immune system supplements.
The effect of diet and nutrition
There's no one-size-fits-all approach to diet. People with inflammatory bowel disease are usually advised to refrain from eating foods that can cause inflammation, such as caffeine, alcohol, some grains, greasy food, refined sugars and others.
Melamed explained that some IBD patients do not follow dietary recommendations since they are made to believe that with the right drug therapy, they can eat everything and anything. This was the theory for decades but not anymore. More and more gastroenterologists are inviting dietitians, nutritionists and coaches into their practice to get involved with creating the perfect diet for people with inflammatory bowel disease.
Keep in mind, though, that certain ingredients and foods can trigger IBD.
"Crohn's and colitis sufferers may find that certain foods exacerbate symptoms and may need to have a special diet," Rhodes said. "Some may find that small changes, like avoiding spicy foods, are enough to manage symptoms, but others may need to make more extreme adjustments, and your diet may change at different times, becoming more restrictive during flare-ups. For example, liquid diets are often prescribed to patients with extreme symptoms. IBD patients should always strive for a balanced and healthy diet. Eating foods high in antioxidants, such as good herbs and spices, oregano, ginger and turmeric, are recommended as well as foods high in omega-3 and omega-6, such as oily fish."
Kaite added that people with inflammatory bowel disease may also need to watch their fiber intake, particularly during a flare-up, as it can worsen gut irritation. The best type of fiber for IBD is soluble fiber, which can be found in cooked apples, oatmeal and ground chia seeds, she said. Soluble fiber soaks up extra fluid in the gut, which helps to slow down digestion and ease diarrhea.
Editor's note: These statements have not been evaluated by the Food and Drug Administration. Our medical experts advise that you consult with your primary healthcare provider before you begin using a supplement. This information is not intended to diagnose, treat, cure or prevent disease.