Fibroadenoma: Recognizing the Realities of Non-Malignancy

Fibroadenomas are common in premenopausal women under the age of 40, but these typically small, benign lumps shouldn't strike panic. There are multiple types of fibroadenomas (which you can read more about here), so variations are normal, and they only very rarely develop into the malignant tumors associated with breast cancer risk.
While the exact cause of fibroadenomas is uncertain, certain circumstances can increase the likelihood of their development or growth, including increased estrogen levels during pregnancy or hormone therapy. Likewise, circumstances that lead to lowered estrogen levels have been found to cause fibroadenomas to shrink or disappear altogether.
You have multiple testing options
Fibroadenomas are usually discovered during a self-exam or a clinical breast exam. They typically manifest as a singular, movable mass with clear definition, though sometimes multiple lumps form in one or both breasts. Despite the relatively low risk associated with these hardened masses, your age, family medical history, level of exposure to dangerous and well-known cancer-causing agents or other factors may cause you or your doctor to seek additional testing to figure out if malignancy is a real concern.
For many people, the logical next step might seem like a mammogram. Other testing options, however, may be better suited to your specific situation—particularly if you fall into a low-risk category for breast cancer. Some of these low-risk categories that should help you breathe easier are if you have little to no family history of cancer, are under the age of 40 and have had minimal exposure to radiation or other cancer-causing agents.
Fibroadenomas are common in premenopausal women under the age of 40, but these typically small, benign lumps shouldn't strike panic.
Mammograms are recommended for women between the ages of 50 and 74, but excessive or unnecessary mammogram screening does come with certain risks, especially since research has shown that the radiation involved with mammograms contains the potential risk of contributing to cancer development in cumulative amounts. Plus, the pressure placed upon breast tissue during a mammogram screening can cause damage, including the rupture of existing tumors.
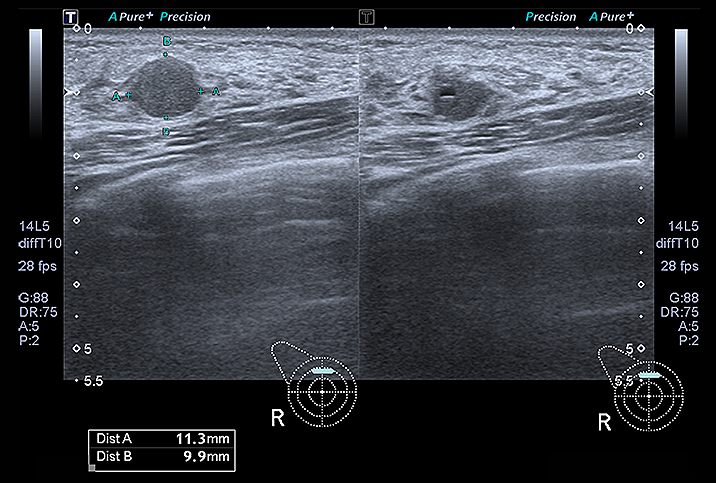
Instead, you might want to talk to your doctor or medical team about getting a better look at the insides of your breasts through options like ultrasound or thermography. Although these procedures may not be covered by your insurance, the peace of mind you'll gain might be worth paying for the out-of-pocket medical care.
Breast cancer is often misdiagnosed
When something changes within the body, it can feel like an abnormality and this can cause a lot of fear and stress. Breast cancer carries substantial risks, so it makes sense that you might want to take every possible precaution, which is why it's important to recognize that the development of non-malignant entities in the body is rarely a cause for alarm.
However, complex fibroadenomas do come with a slight increase in the risk of breast cancer development. Complex fibroadenomas have specific traits that distinguish them from other types, but only about 15 percent of fibroadenomas fall into this category. And even among that 15 percent, the risk is considered slight.
The reality of overdiagnosis and nonessential cancer treatment, though, is hard to ignore. Doctors are prone to exhaustion, oversight and any other number of personal or professional flaws that make them susceptible to mistakes. The medical industry in general is overburdened and healthcare professionals may be prone to overcaution instead of data.
Recently, an artificial intelligence (AI) outperformed six different radiologists in reading mammograms and recognizing cancer. The AI managed to do this without reviewing any data on the medical history of the patients, while the human experts in the same situation had full access to that information. The AI's diagnoses represented a 1.2 percent reduction in false positives and a 2.7 percent reduction in false negatives, or missed cancer incidences, compared to human review.
When something changes within the body, it can feel like an abnormality and this can cause a lot of fear and stress.
However, the AI was only "as good" at accurately reading these images as two doctors working together. This incredibly vital point only stresses the importance of getting a second or even third opinion before taking more drastic steps to treat what may be cancer or a non-malignant entity within the body. While it's a wonderful thing to trust your doctor, you shouldn't trust your doctor so wholeheartedly that you skip a secondary review. Your doctor is, after all, only human.
A few final fibroadenoma facts
If you experience fibroadenoma development, here are a few key things to remember:
- Fibroadenomas are the most common form of benign "lumps" to form in the breast.
- If you're under the age of 30, biopsy of a fibroadenoma is most likely unnecessary.
- Ultrasound is a safe means of viewing the breast tissue for a better understanding of the type of fibroadenoma(s) you've developed.
- Premature or excessive mammography can actually increase the risk of cancer development or non-malignant entities becoming malignant.
- Fibroadenomas are different from, but closely related to, adenomas, which are defined tumors made up of glandular tissue.
- Fibroadenoma removal may be considered for the following reasons: Painful presence in the breast, heightened risk or familial concern about breast cancer development, concerns as a result of a necessary biopsy or for personal reasons, such as the appearance of the breast or discomfort surrounding the presence of the fibroadenoma.
- Removal of a fibroadenoma may result in one or more growing in its place.
Finally, always consult your doctor before taking any potentially unnecessary precautions against what might be a nonharmful development. If there is any reason for speculation as to your doctor's recommendations (and minimal urgency surrounding cancer fears), be sure to get a second opinion from a qualified professional.