You Have Plenty of Treatment Options for Vulvar Cancer

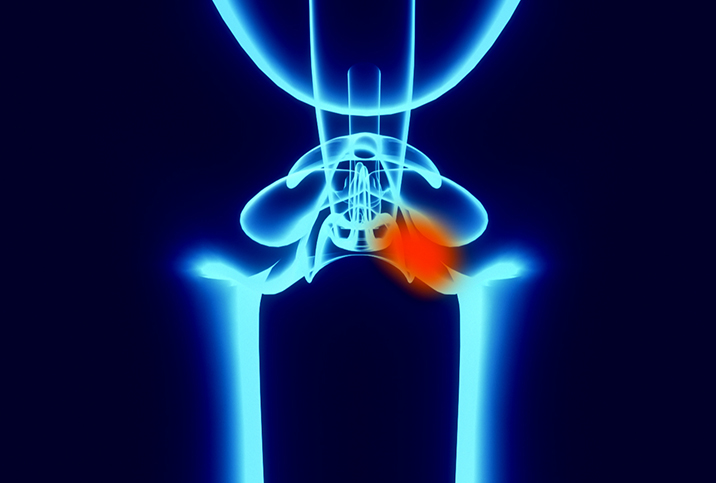
Vulvar cancer affects the external genitalia in females, including the skin and glands around the vaginal opening, the labia minora and labia majora (the inner and outer "lips" surrounding the vagina), and the clitoris, which is the female organ for orgasm.
"Most commonly, this form of cancer mainly impacts the labia, but it can start in the clitoris or the Bartholin glands, which are just behind the labia and they secrete fluids for lubrication during sex," explained Sarah Welsh, M.D., a gynecologist based in the United Kingdom and the founder of the sexual wellness brand HANX.
How is vulvar cancer diagnosed?
Vulvar cancer is usually diagnosed by a doctor examining your vulva, as well as taking your medical history to see if you have any risk factors for vulvar cancer. People older than age 70 are most at risk of vulvar cancer, and people who have had conditions including vulvar intraepithelial neoplasia (VIN), human papillomavirus (HPV) and vulval skin conditions, such as lichen sclerosus, are all at increased risk of developing cancer of the vulva, according to Welsh.
If a doctor suspects you have vulvar cancer, a physical examination typically includes vulvar and pelvic exams.
"This includes looking at the neck of your womb [cervix] with a speculum and feeling your uterus, ovaries, cervix and vagina for anything abnormal," Welsh explained.
If you are referred to a specialist, they may do something called colposcopy, which is where a magnifying instrument is used to view the vulva, cervix and vagina.
"The next step may involve taking a biopsy to the affected area suspecting of vulvar cancer," Welsh said. "This often happens during colposcopy, but if there are large areas or the colposcopy examination is difficult to carry out, you may need to go under general anesthetic for the biopsies to be taken."
From there, the biopsies are examined under a microscope by a specialist pathologist, and this is when cancer can be diagnosed if present.
"Once cancer is confirmed, you will have other tests and scans to assess whether the cancer has spread at all," Welsh said. "These include blood tests, chest X-rays, ultrasound scans, CT and PET-CT scans of the body, MRI scans, as well as proctoscopy and cystoscopy, where a doctor uses a camera to look inside the anus and bladder, respectively."
These tests help the medical professionals looking after you to understand where the cancer started and where (if anywhere) it has spread, allowing them to plan effective treatment.
How is vulvar cancer treated?
The treatment options for vulvar cancer vary depending on the stage and location of your cancer, as well as your overall health. But the main treatment for vulvar cancer is surgery to remove the cancerous tissue.
"This includes surgical excision of the affected area of the vulva as well as any lymph nodes—small structures that are found throughout the body which make up part of the immune system—that contain cancerous cells," Welsh said.
Another option to treat vulvar cancer is removing part or all of the vulva, which is usually done for larger cancers.
"A vulvectomy is a surgical procedure in which the vulva is removed, either partly or completely. This can include removing the labia [minora and majora] and clitoris," Welsh said.
A vulvectomy is sometimes combined with other treatments, like radiation therapy, to shrink the tumor, which may allow for a less extensive surgery.
"Radiotherapy is a procedure that uses high doses of radiation—high-energy particles/waves—to kill and shrink cancer cells," Welsh explained, adding that radiotherapy is usually administered over several weeks using either external radiation, radioactive implants, radioactive liquid [swallowed or injected] or intrabeam radiotherapy [radiation aimed directly at the cancer during surgery], or a combination of these options.
If vulvar cancer has spread to other parts of the body, your doctor might also recommend chemotherapy.
"Chemotherapy drugs circulate the bloodstream and kill cells that are splitting into two. In the case of cancerous cells, they divide and split into two more rapidly than normal cells, so the chemotherapy can target them," Welsh said.
Typically, chemotherapy is administered several times over a few months. However, the number of treatments and length of time are determined by the type of treatment you're having and the extent of your cancer.
Welsh said most chemotherapy is administered intravenously through either a small tube in your hand or arm called a cannula, a peripherally inserted central catheter line (PICC) that stays in place in your arm for a few weeks or months, a central line in your chest that goes to the veins in your heart and stays in place for a few weeks or months, or a small port implanted under your skin.
Some chemotherapy is also taken in tablets. Like radiotherapy, chemotherapy is often recommended alongside surgery to shrink the cancer cells and increase an operation's chances of succeeding.
Targeted drug therapy has been used to treat some cases of vulvar cancer, but more research is required in this area.
"Targeted drug therapy identifies and kills only certain types of cancer cells. Radiotherapy and chemotherapy, on the other hand, can cause damage and death of some healthy cells in the pursuit to eradicate the cancerous cells," Welsh said.
Similarly, immunotherapy is sometimes recommended, especially if you have certain kinds of advanced cancer or traditional treatments are not working.
"There are immunotherapy treatments used to treat vulvar cancer, for example, as a cream that is applied to the skin," Welsh added.
Do you need follow-up appointments after treatment?
Once your vulvar cancer has been treated, you still need to arrange follow-up appointments with your doctor.
"Depending on your circumstances, stage or cancer and the treatments you've had, you will create a follow-up appointment plan with your doctor," Welsh said. "They will only discharge you from the specialist clinic when they feel it is suitable."
At these appointments, you have the opportunity to discuss your healing process, any side effects or any other symptoms you may be having.
"This will allow for the doctors to manage any side effects of the treatments, such as swelling in the genital area and lymphoedema, support you through recovery and pick up any recurrence of cancer as soon as possible," Welsh advised.
You can also ask doctors any questions you have about your recovery at these appointments. With vulvar cancer, the pertinent topics include fertility, sexual function, sexuality and how your body may look after treatment, according to Welsh, and these are all aspects you can discuss with a medical professional.