Symptoms of Vaginitis Can Be Disconcerting but Often Easily Treated

The vagina and vulva are very sensitive, so even slight changes in bacteria levels can make the area the perfect breeding ground for vaginitis.
"Vaginitis is when the vagina has inflammation that may cause a discharge, burning, itching or a bad odor," explained Monte Swarup, M.D., an OB-GYN and the founder of Vaginal Health Hub, based in Arizona.
The symptoms of the disorder can range from mild to severe. And while they are treatable, they should never be ignored.
The different types of vaginitis
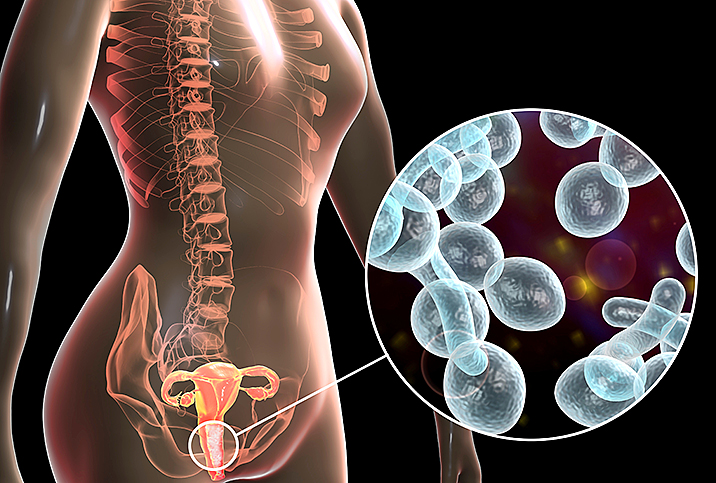
Vaginitis refers to any infection or inflammation in the vagina. The conditions can include atrophic vaginitis, yeast infections, trichomoniasis and bacterial vaginosis (BV).
More than 70 percent of vaginitis cases are caused by BV, trichomoniasis and candidiasis, according to the Journal of the American Medical Association (JAMA) Network.
BV occurs when there's an overgrowth of bacteria in the vagina, whereas candidiasis is caused by a type of fungus called Candida. Bacteria and Candida are naturally found in various parts of the body, such as the gut, mouth and vagina, but simple changes or disturbances in those areas can upset the natural balance.
When that natural setting is thrown off, an imbalance or overgrowth can take hold.
Symptoms of vaginitis
The most common symptoms of BV are pain or itching in the vagina, a foul odor (especially after sex), unusual discharge and burning with urination. Similarly, candidiasis often causes pain or burning during urination, abnormal discharge and vaginal itching.
Some people also experience pain or worsening of symptoms during sex.
While these symptoms can be bothersome, they're not usually a sign of anything serious. However, the disorder still needs to be diagnosed and treated.
Trichomoniasis, on the other hand, is a sexually transmitted infection (STI) that can be passed on to other people. It's estimated that 70 percent of people who have this infection show no signs or symptoms.
If symptoms do present, they may include vaginal burning or itching, pain or discomfort with urination, fish-smelling discharge, or unusual discharge that is green, yellow or thin.
How common is vaginitis?
It's estimated that 30 percent of women experience vaginitis at some point, although that figure could be even higher since some types may be asymptomatic.
BV is the most common vaginal condition and is estimated to affect 29.2 percent of women in the United States between the ages of 14 and 49. While it's more common in women who are sexually active, it also can affect women who are not.
Candidiasis is the second-most common vaginal condition after BV. It accounts for 1.4 million outpatient visits every year.
Risk factors for vaginitis
Vaginitis can be unavoidable for many women, but there are some factors that can put them at higher risk of contracting one of the types. According to Swarup, these factors include the following,:
- Sexual activity
- Douching
- Presence of other STIs
- Hormonal changes
- Antibiotics
- Soaps and other vaginal products
- Genetic susceptibility
Any changes in personal hygiene, sexual partners, bathing products and birth control can make you susceptible to vaginitis. Even if you think your vaginitis was caused by soap or vaginal products, you should still see your doctor for an evaluation to rule out other potential causes and determine the right treatment.
Diagnosis and treatment of vaginitis
Many people with vaginitis don't have any symptoms, so it's likely to be found during a routine gynecological exam. If you do have symptoms, your OB-GYN can take a sample of your vagina's discharge and examine it under a microscope, Swarup explained. They can do further tests to confirm the type of vaginitis.
"It's important to not douche, use spermicides or have sexual intercourse for a few days before your visit," Swarup said.
Treatment for vaginitis varies depending on the cause but often includes creams, pills or vaginal gels. If symptoms aren't relieved, a different treatment might be needed, according to Swarup.
Whether it's due to embarrassment or anxiety, some people try to self-treat vaginal infections at home. This is often done by inserting a tampon soaked in coconut oil or natural yogurt, which is meant to reduce inflammation and replenish good bacteria.
Such measures may work for some people, but they are not recommended.
It's important to be tested so you know what type of infection you have; this allows you to get the correct treatment. Treating your symptoms at home could backfire, leaving you in more pain and discomfort.
Home remedies usually take longer to yield results, whereas antibiotics could relieve most of your symptoms in as little as a few days.
How to prevent vaginitis
Not all vaginitis cases can be prevented, but you can lower your risk by doing the following:
- Avoid douching
- Avoid scented bath products and vaginal products
- Wipe from front to back after a bowel movement
- Wear cotton underwear
- Wash the vagina with warm water only
- Avoid hot water
- Wash after exercising or when you are sweaty
Since vaginitis cannot be completely prevented, knowing the symptoms of the condition and your risk factors for developing it can ensure you see a doctor in a timely manner. Treatment for vaginitis is usually no-invasive—gels, creams, pills—but antibiotics might be necessary, so don't try to make at-home remedies work.