When to Talk to Your OB-GYN About an Ultrasound

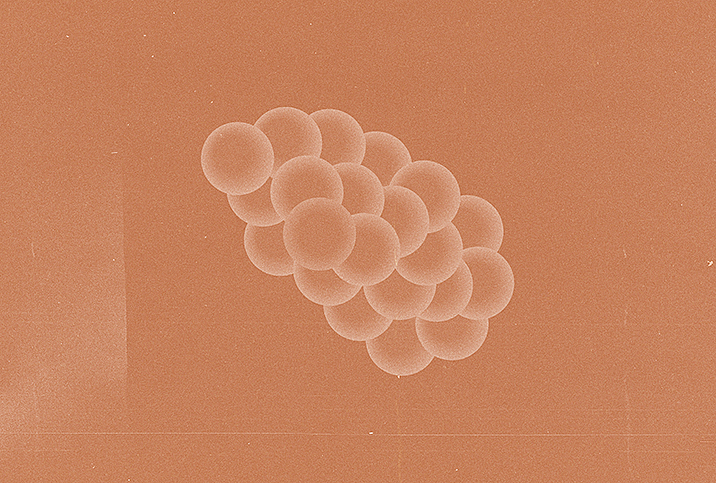
Among the top problems affecting the female reproductive system are uterine fibroids, which are estimated to affect up to 77 percent of women at some point during their childbearing years. Detecting them early is encouraged because it can lead to quicker and more effective treatment options.
One study reported that 30 percent to 35 percent of women are diagnosed with fibroids through ultrasounds, and another study revealed that 21 percent of women who attended an ultrasound and had blood taken were diagnosed with polycystic ovary syndrome (PCOS).
Why your doctor may order an ultrasound
Ultrasounds can play a big role in diagnosing many reproductive conditions. In fact, it remains one of the top diagnostic tools for uterine fibroids, ovarian cysts and adenomyosis.
"Ultrasounds may be ordered for a variety of reasons," said Kiarra King, M.D., an OB-GYN in Melrose Park, Illinois. "When looking specifically at women's reproductive health, if a patient reports symptoms such as pelvic pain, pressure, abnormal bleeding or heavy bleeding, a pelvic ultrasound is usually warranted."
"A pelvic ultrasound is really useful to look at the structure of the cervix, uterus, fallopian tubes and ovaries," explained Dan Nayot, M.D., a reproductive endocrinologist and fertility specialist, OB-GYN and chief medical advisor at Bird&Be, a fertility care company based in Canada. "There is a long list of conditions that it can detect such as ovarian cysts, swollen tubes, fibroids on the uterus or an enlarged cervix."
If a patient notices any sudden changes in their menstrual cycle, such as irregularity, heavy bleeding or painful periods, they should inform their OB-GYN straight away. Other causes for concern are persistent or worsening bloating, fatigue, pain during sex or pain when opening the bowels. If you have any of these symptoms, your doctor will likely order an ultrasound alongside blood tests and a pelvic examination to find the root cause.
What can't be detected via ultrasound
According to Nayot, a routine ultrasound is not recommended as a screening test. While it is often used as an investigative tool, it has some limitations.
"Your doctor may use multiple angles to gather information before reaching a conclusion," he said.
This information includes medical history and finding out when your symptoms started, what triggers them and if anything relieves them. A physical exam is often necessary to check the vulva, vagina, cervix, uterus, fallopian tubes and ovaries. This can reveal any lumps, abnormalities and signs of infection that need further investigation. If the doctor feels it is necessary, they may request bloodwork and imaging; computed tomography (CT) scans and magnetic resonance imaging (MRI) can provide more detail.
Even though an ultrasound is the gold standard when diagnosing many gynecological conditions, it can't be used alone to detect cancer, King said. While cancer could be suspected through an ultrasound, additional testing is required to make a diagnosis and determine the severity of the problem.
Nayot further explained that some gynecological conditions are not large enough to be seen with an ultrasound. For instance, a very early pregnancy cannot be detected on an ultrasound; only a urine or blood hCG test could pick this up. Additionally, if there is a laceration in the vagina, it wouldn't be visible on an ultrasound; this would have to be investigated with a speculum exam.
Can an ultrasound diagnose endometriosis?
Endometriosis is a common reproductive condition affecting around 1 in 10 women, although it's suspected this rate might be higher as many women continue to go undiagnosed. In fact, research estimated that it takes 7.5 years to get an endometriosis diagnosis.
There are many possible reasons for the delay in diagnosis. Nayot said it can be hard to spot the signs of endometriosis, especially if the symptoms are silent, mild or vague. The signs of endometriosis are often mistaken for other conditions, such as irritable bowel syndrome (IBS), since bowel issues are a very common part of the condition.
King said one surprising reason that endometriosis goes ignored for so long is that some women think extreme period pain is normal.
"They suffer in silence because they believe that's what their bodies are supposed to do," King said.
Lack of awareness in schools and professional settings is partly to blame for this shortcoming, along with the ideology that women are expected to cope with period pain because it's "natural." The best thing that women can do is to be their own advocates and speak up about any new or worrying symptoms they have.
One way to investigate endometriosis is with an ultrasound, but King explained that there are limitations.
"Studies like ultrasound are most useful if ovarian involvement, [that is,] an endometrioma, is present," King said. "So if there is involvement of the bladder or rectum, those lesions may not be detected on ultrasound."
If an ultrasound comes back clear, this doesn't rule out endometriosis indefinitely. King said the only way to get a definitive diagnosis is through testing a piece of tissue, which is typically done at the time of diagnostic laparoscopy. Therefore, if your symptoms persist or worsen, you should consider asking your doctor for a laparoscopy.