How Can I Have an STI? I Have No Symptoms!

Sexually transmitted diseases (STDs) are on the rise. They have continued to increase over the past few years, and the Centers for Disease Control and Prevention (CDC) recently reported 2.5 million documented cases of chlamydia, gonorrhea and syphilis in 2021 in the United States.
This represents just a small portion of the total number of sexually transmitted infections (STIs) in the U.S. In 2018, the CDC reported that the total number of STI infections reached 26 million.
Although the terms STI and STD are often used interchangeably, they are not the same. A way to tell them apart is to know that all sexually transmitted diseases are preceded by a sexually transmitted infection, but not all STIs result in the development of an STD.
The problem is it's not always easy to know you have a sexually transmitted infection because they don't always present symptoms—even the more serious infections.
Which STIs sometimes don't show any symptoms?
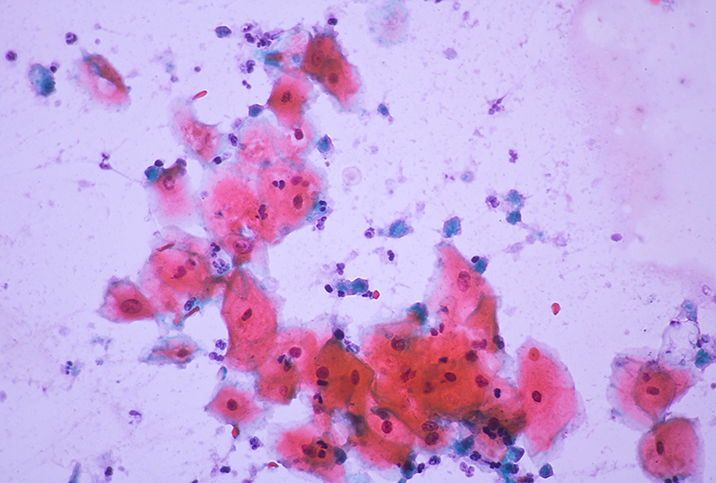
"Human papillomavirus [HPV] is the most common STI without symptoms: Up to 80 percent of sexually active people catch it at some time in their life," said Shazia Malik, M.B.Ch.B., a consultant obstetrician and gynecologist on behalf of Balance Activ, a leading women's intimate healthcare brand in the United Kingdom.
However, Monte Swarup, M.D., a board-certified OB-GYN in Arizona and founder of the HPV Hub information site, added that many STIs and STDs are asymptomatic and show no signs or symptoms at all, including the following:
- Chlamydia. In its early stages, it is often difficult to detect symptoms.
- Gonorrhea. This STD is a genital tract bacterial infection. Symptoms usually do not appear until 10 days after you are exposed to it. Sometimes people can be infected yet not show symptoms for months.
- Hepatitis A, B and C. These are contagious viral infections, and some people never develop symptoms.
- Herpes. The herpes simplex virus (HSV) enters through small mucous membranes. Most people have no symptoms, so it often goes unnoticed and unreported.
- HIV. When first infected, you have no symptoms at all.
- HPV. One of the most common STIs and one that puts women at risk for cervical cancer. HPV usually has no symptoms and most often clears up within two years without anyone knowing.
- Syphilis. This STD affects the nervous system, but there are few symptoms in the early stages for most cases and the issues go away if untreated, although the disease can return sometimes years in the future.
- Trichomoniasis. Trichomonas vaginalis, a microscopic parasite, causes "trich" and spreads through intercourse. It infects men's urinary tract but often causes no symptoms.
What should you watch out for?
Obviously, you can't spot symptoms that aren't present. However, Malik advised paying particular attention to any unusual symptoms such as painful sex, discharge from the vagina or penis (especially if it has a distinctive odor), burning when passing urine, spotting between periods, pelvic pain or a high temperature.
You should especially take note if you've had sex without a condom and any of these symptoms present.
Swarup added that for hepatitis, even weeks after close, personal or sexual contact, you may notice symptoms that you might not associate with an STI, such as:
- Appetite loss
- Fever
- Itching
- Muscle pain
- Nausea
- Pain in the abdomen
- Skin yellowing or jaundice
- Vomiting
If you have no STI symptoms but are sexually active, you should still get tested regularly because any kind of sexual infection can cause major problems if left untreated and, of course, may get passed on through further sexual encounters.
What happens if you don't get treated?
Just because an STI presents no symptoms doesn't make it less serious.
"If you don't get treated and you have an STI, you're at risk of getting another STI because your immune system may be compromised," Swarup explained. "STIs can also cause sores and stimulate a response of your immune system, raising your risk of transmission."
More importantly, he noted that untreated STIs could lead to organ damage, certain types of cancer, infertility and even death.
Malik added that HPV is the leading cause of cervical cancer in women.
"STIs can also damage your pelvic organs and affect your future fertility and your chances of having a natural family," she added. "In fact, damage to your fallopian tubes can even cause you harm if you do get pregnant by increasing the risk of a pregnancy implanted outside the womb."
This occurrence is called an ectopic pregnancy and makes the pregnancy nonviable, resulting in a rupture and causing life-threatening bleeding inside your stomach
If I have no symptoms, do I need an STI test?
"If you're sexually active—if you have oral, vaginal or anal intercourse or touch the genitals of a partner—you can get an STD or STI, thus, you should get tested regularly," Swarup said.
"It's advisable to get an STI test at least once a year," Malik recommended. "And definitely more often if you have a new partner. And make sure they get tested, too."
She added that if you have more than one sexual partner, make sure you and they get tested more often—symptoms or not.
The STI screening recommendations from the CDC are as follows:
- People ages 13 to 64 should be tested at least once in their life for HIV.
- People younger than 25 should be tested for gonorrhea and chlamydia once a year.
- People older than 25 with new or multiple sex partners or a sex partner who has an STI should also get tested for gonorrhea and chlamydia annually.
- Everyone who is pregnant should be tested for syphilis, HIV, and hepatitis B and C. Those at risk for infection should also be tested for chlamydia and gonorrhea.
- All sexually active gay, bisexual and other men who have sex with men should be tested:
- At least once a year for syphilis, chlamydia and gonorrhea, and more frequently if you have multiple partners.
- At least once a year for HIV and may benefit from more frequent HIV testing.
- At least once a year for hepatitis C, if living with HIV.
- Anyone who engages in risky behavior that could lead to infection, such as needle sharing, should get tested for HIV at least once a year.
- People who have had oral or anal sex should talk with their healthcare provider about throat and rectal testing options.
If you're wondering whether you should get tested, the best judgment call is to test. It's quick and easy, and when you get a clean bill of health, you'll feel more confident and stress-free.