A Closer Look at the Secondary Stage of Syphilis
In 2021, syphilis cases increased by 26 percent over the previous year in the United States, the highest spike in three decades. Infection rates for primary and secondary syphilis have risen to an estimated 15.8 per 100,000 individuals.
The bacterium Treponema pallidum causes syphilis, which can be identified through skin lesions, rashes and other symptoms. However, if this sexually transmitted disease (STD) goes unrecognized, the severity of the condition increases with each subsequent stage. Without treatment, primary syphilis can develop into further stages of infection, starting with secondary and then, if left untreated, progressing into latent and tertiary stages.
Although the primary and secondary stages of syphilis are curable with treatment, preventing progression to the tertiary stage is important. Later stages of infection may not be curable and generally result in organ damage, dementia, paralysis and even death.
What is secondary syphilis?
Syphilis transmits through broken skin or mucus membranes. The most common way syphilis spreads is through sexual contact, including vaginal, oral or anal sex without a condom. However, sharing unwashed sex toys or genital touching—even without penetration, orgasm or ejaculation—can also spread infection. Additionally, syphilis can be passed to a baby during childbirth or pregnancy if the birthing parent is infected.
Typically, symptoms present within 21 days of contraction. However, symptoms can manifest anytime within a 10- to 90-day period.
The first sign of syphilis is a papule, a solid, raised bump. Syphilis papules often form a rash but also can form into an ulcer or chancre, and are highly contagious. Typically, chancres form on the penis, labia, cervix or rectal region. Chancres inside the vagina are more likely to go unnoticed.
Since secondary syphilis can affect individuals differently, rashes can be difficult to notice.
Sasha Haddad, D.O., a resident at Northridge Hospital in California, noted secondary syphilis often goes untreated because symptoms may not be easily identifiable.
"One of the most common misconceptions is if you have a sexually transmitted infection [STI], you will know because it would be obvious. False!" Haddad explained. "Symptoms can be vague or you may not notice any concerning symptoms at all. If secondary syphilis goes untreated, your symptoms might seem like they've gone away, but you can advance the latent form of syphilis."
About 1 in 4 individuals with untreated primary syphilis develop secondary syphilis six to 12 weeks after primary infection. However, identifying various secondary syphilis symptoms can alert you to visit your doctor and get treatment to prevent progression into the latent stage.
Changes in secondary syphilis
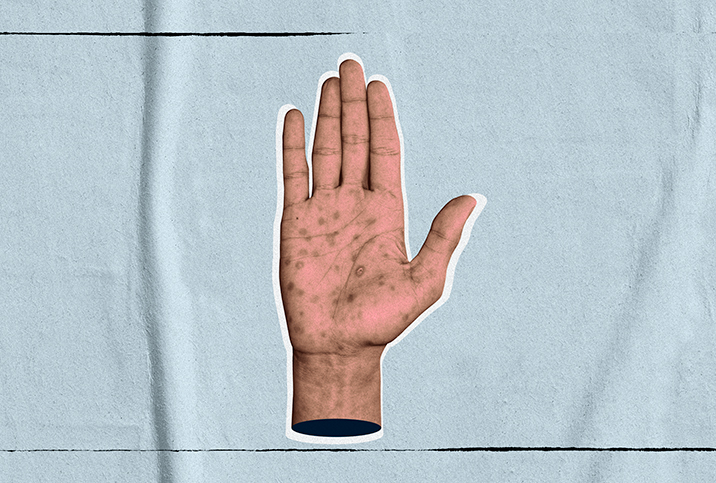
Criteria of secondary syphilis include skin rashes and lesions in the mouth, vagina or anus. These rashes and lesions appear after the chancre has developed or before it heals.
Rashes usually do not cause itching and may appear as rough red or brown spots on the palms or bottoms of the feet. However, rashes can appear in other areas of the body. Small, open sores can be present on mucous membranes, such as the throat, mouth, urethra, rectum and vagina.
Additional signs of the secondary stage include sore throat, headache, weight loss, low-grade fever and muscle aches. Nervous system symptoms can include irritability, paralysis, unequal reflexes and irregular pupils.
Since secondary syphilis affects individuals differently, symptoms may go unnoticed. Additionally, sores on mucous membranes may be asymptomatic. However, it's important to note the secondary stage of syphilis is very contagious.
Tests for syphilis
Testing for the Treponema pallidum bacterium and diagnosing syphilis can include dark-field microscopy, nontreponemal tests and treponemal-specific tests.
Dark-field microscopy is the most common test for diagnosing syphilis when there is an active chancre present. The process includes abrading the chancre and then testing the tissue for bacteria.
Nontreponemal tests include testing for the production of nonspecific antibodies that react to cardiolipin, an important component of the inner mitochondrial membrane. However, the usefulness of the exam decreases during early primary syphilis and late syphilis, specifically, when one-third of people tested may not show any symptoms.
Treponemal-specific tests detect antibodies that are associated with syphilis. The treponemal test can identify individuals who were previously treated for syphilis and those with untreated syphilis.
Treatment options
Secondary syphilis undergoes the same treatment process as primary syphilis.
Penicillin is a highly effective treatment option to cure lesions during primary and secondary syphilis and prevent progression to the latent stage. Additionally, doxycycline and oral azithromycin can be administered to treat and prevent infections.
Unlike secondary syphilis, latent syphilis may not show any symptoms.
Madeline Sutton, M.D., a board-certified OB-GYN based in Stone Mountain, Georgia, explained the shift to latent syphilis.
"When secondary syphilis is untreated, it becomes latent syphilis," she said. "There are no visible signs or symptoms during the latent syphilis phase. This stage can last for years. However, syphilis can still be treated and cured even if diagnosed at this latent stage."
Further management of syphilis includes clinical evaluation to ensure treatment options have eliminated symptoms. Individuals who have syphilis are at risk for reinfection, so regular screening is recommended even after initial diagnosis.
According to the Centers for Disease Control and Prevention (CDC), sexually active individuals should receive STI/STD testing at least once a year. For individuals with multiple or anonymous partners, testing should be more frequent: every three to six months.
"A big misconception is that you can look at a potential sex partner and tell if they have syphilis," Sutton said. "Syphilis can look like many other things, and sometimes people can be unaware of certain symptoms. So never assume. Condoms and/or knowing baseline [STI] status are good prevention strategies."