A Deep Dive Into Prostate Biopsies

At just 4 centimeters wide, the tiny prostate gland may seem far too small to pose such a formidable health threat to hundreds of thousands of males from year to year. But prostate cancer is the second-leading cancer (after skin cancer) in men, and it is a prolific killer. The American Cancer Society anticipates more than 34,000 deaths due to prostate cancer in 2021 and estimates that 1 in 8 males will be diagnosed with the disease in their lifetime.
Those are sobering numbers even if you're not at high risk for prostate cancer, and even the most hardened skeptic can't help but recognize the importance of prevention. Cancer screening is a fairly simple matter these days, but the process can get quite complicated when a prostate biopsy is indicated.
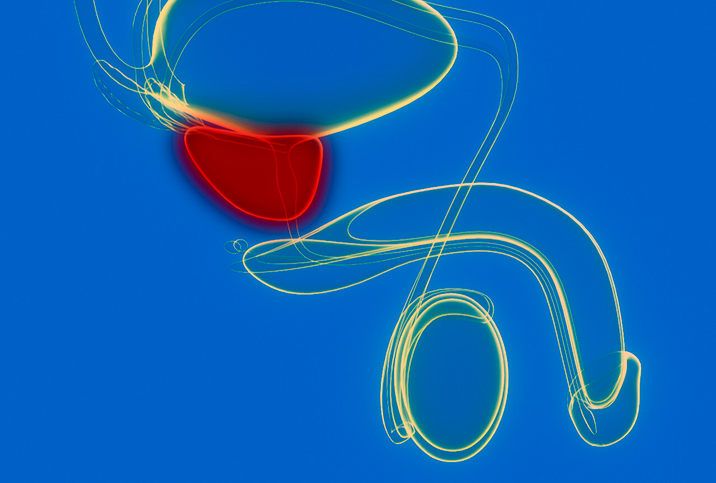
A biopsy is the removal of a sample of tissue or cells from the body for testing. It is generally recommended when a doctor finds abnormalities during a digital rectal examination (DRE), when prostate-specific antigen (PSA) levels are unusually high or when abnormal prostate cells are identified. The prostate isn't the most easily accessible organ, wedged between the rectum and the bladder. Fortunately, several methods using high-tech ultrasound guidance to gather tissue samples are highly productive for performing a prostate biopsy.
Transrectal ultrasound
Transrectal ultrasound-guided systematic biopsy is often considered state of the art for diagnosing prostate cancer. The patient lies on his left side, and an ultrasound probe about the width of a pencil is inserted into the rectal opening. Guided by the probe, anesthesia is injected into tissue surrounding the prostate and once the entire space is numb, ultrasound guidance enables tissue samples to be obtained from as many as 18 areas using a 17-millimeter-long needle.
A transrectal ultrasound (TRUS) is a popular option because the patient can be in and out in about 20 minutes. However, it should be noted that this approach is also known for its low sensitivity and a false-negative rate—showing no cancer when cancer is present—as high as 35 percent.
Transperineal biopsy
Transperineal biopsy offers physicians a somewhat more minute, systematic alternative for examining the prostate and, consequently, it is more accurate in biopsying difficult-to-reach parts of the walnut-sized gland. That's significant because approximately 25 percent of prostate cancer cases arise in the transition zone, which surrounds the part of the urethra that passes through the prostate, while about 10 percent occur in the anterior zone, where a TRUS biopsy is least effective.
Once the prostate size and volume have been assessed with an ultrasound probe, an 18-gauge needle is inserted through an incision made in the perineum and into the prostate, where multiple tissue samples are gathered from at least two dozen sites. Transperineal biopsy offers easier access to the prostate and, because the needle doesn't go through the rectum, there is a lower risk of infection (the risk of sepsis with transperineal biopsy is 1 in 500). The prostate can also be biopsied via the urethra, the narrow tube that carries semen and urine to the penis. This method involves the insertion of a cystoscope, a tiny camera that captures images of the prostate while tissue samples are gathered from the prostate through the urethral wall.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) can be used in combination with ultrasound to examine targeted parts of the prostate and guide the needle into the organ. This method is often more accurate and requires fewer biopsies to be performed. Of particular importance is that this method makes it possible to identify aggressive, harder-to-reach lesions, which aids detection and can produce higher rates of survivability.
Prostate cancer can only be diagnosed from a tissue sample, so the accuracy of any biopsy procedure is paramount, especially in an organ as small as the prostate. Ever-improving technologies, such as ultrasound and MRI, offer the potential for better, more targeted diagnoses, more timely treatment and, hopefully, more prostate cancer survivors.