Millennial Moms Are Having Postpartum Sex Before They're Ready

Postpartum recovery can be fraught with challenges, namely, taking care of a brand-new, helpless little human around the clock as your own body recovers from possibly the most physically and emotionally challenging endeavor of your life. You'd think the last thing on your mind would be your sex life. But in a 2019 Motherly survey of millennial moms, 31 percent of respondents reported having postpartum sex before they were ready.
At the six-week postpartum appointment, if all goes well, the OB-GYN typically clears mothers to return to sex. But just because they have been physically cleared doesn't mean they are healed enough to jump right back in where they left off, or that they are emotionally ready to have sex again. Thirty-eight percent of moms in the Motherly study even reported it took six to 12 months before they were interested in sexual intimacy again.
Women should be really ready before hopping back in the sack for anything other than a much-deserved nap. So why are moms pushing themselves to recover faster than feels natural to them?
Partners are pushing them to do it
Many forms of partner pressure might make a birthing person have sex before they really want to have it. Partners might not say anything but instead nonverbally indicate they want to have sex. They might ask for it outright or make advances suggesting that's their hope.
"I have found postpartum patients tend to express wanting to wait longer to attempt sex than their partners," said Alexis May Tran Kimble, OB-GYN and urogynecologist at the Kimble Center for Pelvic Wellness in Los Angeles. "I have seen partners who have been ready and willing to initiate sex or sexual activity even the same day after delivery."
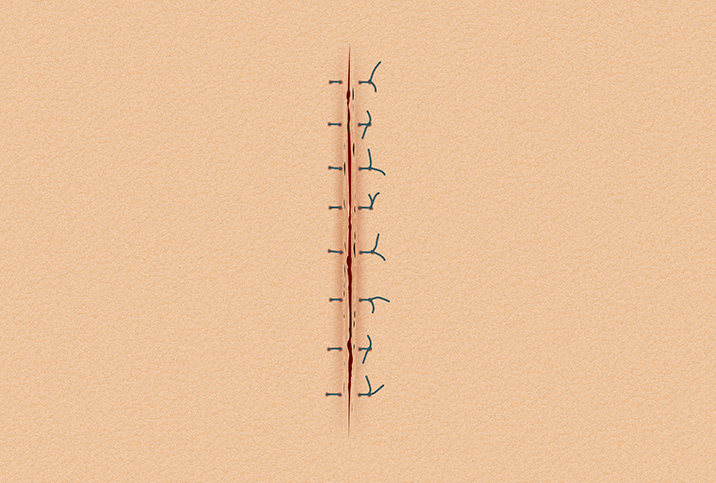
Not only can sex be harmful, but it can cause serious medical complications. Kimble said the vaginal bleeding and cramping that occur after birth need to have stopped completely, and any incisions need to heal. In addition, postpartum patients with large clots or debilitating pain might have complications such as retained placenta, uterine infection or postpartum hemorrhage. That six-week appointment isn't random timing, but an intentional and necessary checkup that certainly doesn't just mean it's now OK to have sex.
"Being ready to have sex after delivery differs from when it is simply safe to do so," she said.
Moms are pressuring themselves
People have sex for a variety of reasons that don't involve actually getting pleasure, Kimble explained. For example, you may desire to get closer to your partner in a time of transition or desire some semblance of normalcy, she said. For some moms, the pressure isn't actually from their partner but from within themselves, especially if they feel the partner has waited a long time, such as through the end of pregnancy months and the early postpartum period.
Sonia Wright, a radiologist, sexual counselor and life coach in the Minneapolis-St. Paul area and medical advisor at the Body Agency, said society's conception of a "good woman" mistakenly assumes she should focus on everybody else. Instead, it's important and necessary for moms to reconnect with their body and recognize what they need spiritually, emotionally and physically, Wright said.
They see their bodies as there for others' pleasure
If a postpartum mom knows she doesn't want to have sex but also knows her partner does, she might defer to their wants over her own, an issue that starts in our society long before the postpartum time period, Wright said.
"It's important to talk to our girls and have them understand from a young age that their body is important and they have ownership of their body, and that they're there for themselves and not necessarily for other people's pleasure," she explained.
It's the perfect time to set boundaries and take care of your own recovery first.
"I see that the behaviors adopted following delivery can set the stage for long-term behaviors and attitudes toward sex and one's partner," Kimble said.
Wright said women disconnect from their bodies when they cause pain, dating back to their first menstrual cycles. She hopes postpartum women listen to their own bodies if they are communicating postpartum pain in general or during sex, instead of pushing through for others.
Paths parents can take
Postpartum parents who are encountering issues with returning to sex have many options and don't have to just endure discomfort.
A PLOS One study from April 2021 revealed that 31 percent of perinatal participants reported anxiety or depression, 53 percent were lonely, and 43 percent had post-traumatic stress related to COVID-19 life. Piling pandemic stressors on top of an already difficult and sleep-deprived period can make new parents vulnerable to serious mental health challenges—but your doctor can help.
"When postpartum parents are faced by the many changes posed by a new baby and unable to shake feelings of being overwhelmed at the many new things that need attending, feel alone, isolated or sad or when usual things that are enjoyable have seemed to lost their luster, it may be time to revisit the OB-GYN to determine if this is not a fit of the blues or more concerning postpartum depression," Kimble said.
Treating postpartum depression and anxiety can help you return to your normal sex life.
Acknowledging body changes is also key. Nobody really feels their hottest during sleep-deprived postpartum days when the messy bun and coffee breath rule.
"New moms may not necessarily feel sexy soon after delivery," Kimble said. "While the body is able to withstand many of the stresses of pregnancy and birth no matter the route of delivery, the self-consciousness related to changes in body morphology, like a scar or pendulous abdomen, active lactation or the vagina appearing larger or wider, can affect how sexy a woman feels and can be very discouraging."
It can help to focus on what your body accomplished and to communicate with your partner about your body's changes and how they make you feel. You might find they love your body even more than your pre-baby body. If body image continues to be a struggle, consider seeking help from a postpartum therapist who can give you strategies. Kimble added that pelvic floor therapy can help with rehabilitating the vagina for increased comfort during sex and your OB-GYN can refer you to a therapist.
A woman can be both a mother and a sexual being, a perception Wright hopes more women can adopt. "There's no magic day on the calendar to begin [having sex]," she noted.