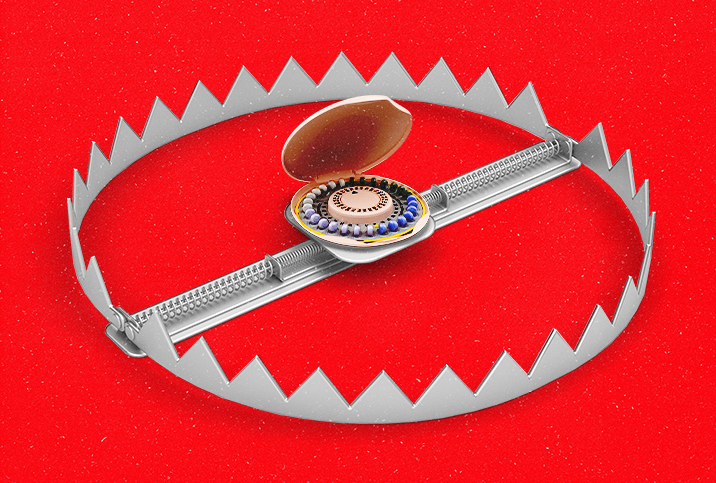
The Connection Between Migraines With Aura and Birth Control

If you've ever had a migraine with aura, you know how downright uncomfortable they can be—and if you haven't, you're very lucky.
If you take hormonal birth control, you might be unaware that your contraceptive could increase your risk for migraines. What do migraines with aura and birth control have to do with each other? We talked to the experts to find out.
Defining a migraine with aura
"A migraine with aura is where you experience certain symptoms before a migraine begins, effectively warning you that you're about to have a migraine," said Sam Wild, a general practitioner, women's health clinical lead and primary care physician at Bupa Health Clinics in London. "You might have changes to your vision like seeing flashing lights, zigzag patterns or blind spots. Alongside the changes in sight, you might have numbness, tingling, muscle weakness or dizziness."
Kecia Gaither, M.D., director of perinatal services at NYC Health + Hospitals/Lincoln in the Bronx in New York City, described a migraine as a "severe throbbing headache" and said aura involves sensory disturbances, such as those described by Wild, coupled with possible nausea and vomiting.
Migraines with aura can be unnerving because they might mimic stroke symptoms, said Alyssa Dweck, M.D., a medical advisor in Mount Kisco, New York, for Intimina, a women's health products company.
Migraines with aura not only mimic stroke symptoms but also increase your risk factor for stroke.
"If you have migraine with aura, you're about twice as likely to have an ischemic stroke—a type of stroke caused by a blockage in an artery that supplies blood to the brain—in your lifetime compared to those without migraine," said Shivani Dattani, M.B.B.S, a GP at London Gynaecology. "However, the overall risk linked to migraine is still very low, and you are far more likely to have a stroke because of other risk factors like smoking and high blood pressure."
The link to birth control
The connection between migraines with aura and birth control lies in the combined hormones found in hormonal contraceptives.
The combined oral contraceptive pill, the contraceptive vaginal ring and the contraceptive patch all contain the hormone estrogen and are called combined hormonal contraceptives (CHCs), Dattani said.
"Estrogen is used in birth control at higher than naturally occurring levels to prevent ovulation and, thus, pregnancy," said Betsy Greenleaf, D.O., a physician in Howell, New Jersey, owner of the Pelvic Health Institute at Greenleaf Health and Wellness and CEO of the Pelvic Floor Store. "When estrogen levels are higher, women tend to be less susceptible to pain, however, when estrogen drops due to normal cycling of hormones, placebo pills in the oral birth control, pregnancy or menopause, susceptible women can be more at risk of pain syndromes such as migraines."
Essentially, if you're taking a CHC with a monthly gap and noticing a migraine around the same time each month, it's potentially due to your birth control.
"Combination birth control keeps the estrogen at a steady state, but when a woman reaches the end of the pack, either low-estrogen or placebo sugar pills are used for the last week, thus, significantly dropping estrogen levels and increasing the risk of migraine," Greenleaf confirmed.
The risk of stroke
"[The risk of stroke] is thought to be related to the increased clotting risk associated with estrogen that can lead to an ischemic stroke," said Amina Albeyatti, M.B.B.S, M.R.C.G.P., a general practitioner at the Private GP Group in London.
Greenleaf broke this down further: "Individuals with migraines have a risk of stroke. Birth control increases the risk of migraines. But as much as we want to go back to high school math class and say if A equals B and B equals C, then A equals C, we just can't make that connection absolutely at this time.
"We do know that individuals that suffer migraines have a risk of vascular abnormalities increasing the risk of stroke," she continued. "The use of birth control in a person that has migraines should be an individual decision between a person and their doctor, however, in my opinion, I would want to investigate other options for birth control that does not include hormones."
"Although this stroke risk is very small, your risk increases further if you experience migraines with aura alongside taking the pill or using the patch or ring," Wild added. "It's not clear why ischemic strokes are linked to migraine, [but] if you get migraines with aura, it's important to talk to your doctor so they can assess your stroke risk and discuss alternative forms of contraception that are safer for you."
What the research says
The link between migraine with aura, birth control containing estrogen and stroke has been discussed and studied for several years.
"A preponderance of evidence suggests that migraine, particularly migraine with aura, is associated with an increased risk of ischemic stroke, and that this risk may be further elevated in the setting of combined estrogen-progesterone contraceptive use," stated the authors of a 2010 review published in Reviews in Obstetrics and Gynecology.
The American Headache Society (AHS) states on its website: "The presence of migraine with aura is known to increase the risk of stroke, especially in women, and research has also shown that the use of combined oral contraceptives…is linked to a higher risk of stroke as well."
Taking a look at a systematic review
The AHS also pointed to a 2017 systematic review in the journal Headache that looked to establish whether there is, indeed, a synergism between migraine and combined oral contraceptives related to stroke risk, and how the two factors correlate. Huma U. Sheikh, M.D., a board-certified neurologist with a subspeciality in headache medicine in New York City, was the lead author.
"I decided to do this review because there was a lot of confusion regarding the use of estrogen-containing contraceptives in women who have migraine," Sheikh said. "There is concern that estrogen can increase rates of clots and stroke when added in women who have migraine. Migraine itself can be a risk of stroke, and there are older studies showing that exogenous estrogen can be another risk factor. We felt that it was an important study since so many young women have migraine and many of them are in their reproductive years who need a form of birth control."
When Sheikh began her research for this review, she was struck by the lack of data available.
"The studies looking at whether estrogen affects women who have migraine were very old," she said. "The doses of estrogen in these studies were much larger than what we use now and, therefore, it was difficult to assess whether they were even valid in this day and age."
Unfortunately, the review also found current research was lacking: "Studies were generally small and confidence intervals were wide…This systematic review shows a lack of good quality studies assessing risk of stroke associated with low-dose estrogen use in women with migraine. Further study is needed."
Sheikh said the research gaps have not improved over the past five years since the review was carried out.
"We tried to do an updated review in the last couple of years, but there was no new data to look at," she said.
The review concluded: "The available evidence is consistent with an additive increase in stroke risk with CHC use in women with migraine with aura."
Sheikh confirmed the data showed this, but she added a caveat: "This is with the higher doses of exogenous estrogen that were used in the studies…Today, we use much lower doses of exogenous estrogen, so this information may not necessarily still hold true."
Overall, both the review and Sheikh confirmed that the overall risk of stroke from combined hormonal contraceptives is still low.
"The decision to take exogenous estrogen should be made on an individual basis," Sheikh said. "There are a number of factors to keep in mind, including what the estrogen is for, whether it is [for] a medical condition versus for pregnancy prevention.
"The risks of not using the birth control should also be taken into consideration, since pregnancy also has risks of medical issues, including stroke," Sheikh continued. "If someone has migraine with aura and is a smoker, then I would highly recommend not using exogenous estrogen."
Alternative forms of contraception
"The risk [of stroke] is only present within the combined contraceptive pill that contains a derivative of estrogen and progesterone and not the minipill, which only contains progesterone," Albeyatti said.
Therefore, progesterone-only options, such as the implant, could be an alternative form of contraception for someone prone to or who has recently developed migraines or migraines with aura.
Gaither suggested the copper IUD, barrier options such as the diaphragm or condoms, or the rhythm method for anyone who's been advised by a healthcare professional not to pursue estrogen-containing contraception.
It's also worth noting that migraine without aura isn't generally dangerous for birth control users.
"If you suffer with migraine without aura, then you can usually use combined hormonal contraception safely unless you have other [stroke] risk factors, such as high blood pressure or a family history of heart disease or stroke," Wild said.
Treating migraines
As for the migraines themselves, Wild suggested using over-the-counter painkillers, triptans and anti-sickness medication if the symptoms are relatively infrequent. If they occur regularly, Wild advised speaking to your doctor about preventive treatment such as medication you can take daily to reduce migraine frequency and severity.
"It can also be useful to review your lifestyle to see if there are any changes that can be made to reduce your chance of migraine attacks, like increasing your sleep or reducing the amount of alcohol you drink," Wild said.
As always, you should see your doctor if you experience migraines with aura, especially if you're taking a form of CHC.
"If you get your first-ever migraine with aura after starting a combined hormonal contraceptive, then please see your GP as soon as possible to get this reviewed," Wild concluded.