Maintaining a Healthy Cervix Isn't Complicated

It's fair to say many men don't know what the cervix is or what it does. It's also fair to say a good number of women don't know what the cervix is or what it does, according to a survey conducted by Jo's Cervical Cancer Trust in the United Kingdom. Fully 44 percent of women were unaware of what the cervix is, and 1 in 6 could not name a single function of the organ.
The cervix is the lower portion of the uterus that connects to the vagina. This organ plays multiple key functions in reproductive health: it keeps harmful bacteria out of the uterus, cleans the vagina, allows menstrual blood or sperm to pass through, and has a vital role in fertility, pregnancy and labor. For some people, the cervix can also be a source of pleasure.
Each year, almost 14,000 new cases of cervical cancer are diagnosed in the United States and about 4,300 women die of the disease. According to the World Health Organization (WHO), cervical cancer is the fourth-most common cancer among women globally. January might be Cervical Health Awareness Month, but no time is a bad time to raise awareness about cervical cancer and the power of timely screenings.
Through early treatment and screening, cervical cancer is one of the most preventable cancers. There are plenty of ways to reduce the risk of cervical cancer and keep your cervix healthy. Early detection and intervention are vital to detecting precancerous cells and stopping them before they turn cancerous.
STIs and cervical health
Human papillomavirus (HPV) is an extremely common sexually transmitted infection (STI): Around 80 percent of women in America get it by age 50. Many people with HPV are asymptomatic, and it's common for people to be unaware they have the infection. For these reasons, it can be easily spread.
For people with cervixes, certain types of HPV can be harmful if left untreated. Of the more than 100 types of HPV, 13 types can lead to cervical and other cancers, according to the International Agency for Research on Cancer.
Almost all cervical cancer cases—95 percent, according to the WHO—are caused by HPV. However, 90 percent of people with HPV clear the infection on their own. Just because you have an HPV infection does not mean it will turn into cancer; in fact, many types do not cause cervical cancer at all. Types 16 and 18 are responsible for nearly 50 percent of high-grade cervical precancers.
In addition to HPV, other STIs can also bring harm to cervical health, causing inflammation and infection of the cervix and the uterus, said Beri Ridgeway, M.D., a board-certified OB-GYN in Cleveland and a co-founder of Ina Labs, creators of skincare and feminine hygiene products. Untreated chlamydia and gonorrhea can cause pelvic inflammatory disease (PID), an infection of the upper genital tract, including the cervix. PID can cause harmful and lasting effects such as infertility and chronic pain.
The significance of routine screening
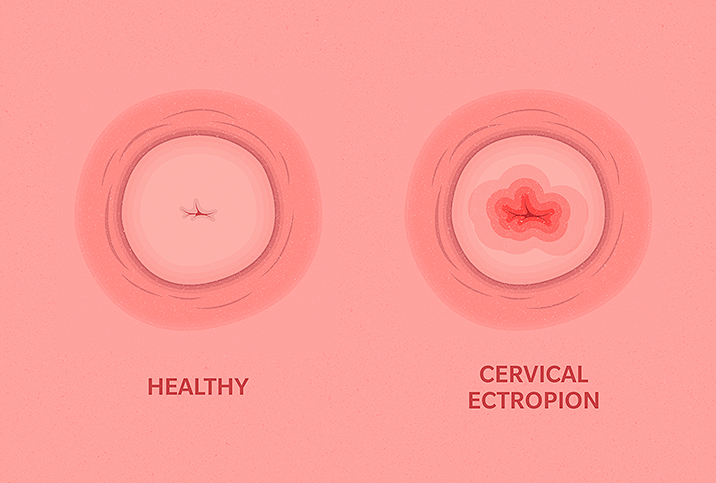
Routine screening is a simple yet lifesaving intervention. The sooner an infection is detected, the sooner someone can receive treatment. During a Pap test, a provider uses a small brush to collect cervical cells to screen for precancerous cells that could become cancerous if left untreated. Recommendations on how often someone should receive a Pap test depend on age and personal history, Ridgeway said.
Separate from Pap tests, people who are sexually active should receive STI testing once a year, or every three to six months if the person has multiple sexual partners, according to Monica Grover, D.O., an OB-GYN and the chief medical officer at VSPOT, a women's intimate health platform in New York City.
Recommended guidelines concerning the frequency of Pap tests and STI tests are different, though.
"Pap screenings can often be confused with well-woman exams," Grover said. "Pap screenings can be every three years for ages of 21 to 29; and from 30 to 65, either a Pap test every three years, an HPV test every five years, or Pap and HPV every five years."
The risk for HPV can decline with age, but cervical cancer is still possible. According to the Centers for Disease Control and Prevention (CDC), someone should have at least three normal Pap tests in a row before stopping screening after age 65. Other risk factors, such as a weakened immune system, can help determine individual screening needs.
"After 65, an educated decision between the doctor and the patient can be made as to how often a screening test should be," Grover said.
Other screenings after age 65 are still vital, though.
"A woman should still see her OB-GYN annually for a well-woman exam that would include a breast exam, a pelvic exam, STI testing and contraceptive counseling, along with other concerns," Grover said.
Lifestyle recommendations to keep your cervix healthy
Practicing safer sex is vital to cervical health. Condoms and latex barriers can help prevent sexually transmitted infections, such as gonorrhea, chlamydia, trichomoniasis and HPV, that can affect the cervix, according to Grover.
An imbalanced vaginal pH can increase the risk of infections, including STIs.
"Recurrent bacterial and yeast infections can also cause cervical issues, so it is important to be treated for those in addition to maintaining an optimal vaginal pH of around 4.5," Grover said.
Lifestyle changes such as eating more alkaline foods, decreasing stress and not douching can all benefit pH balance.
Dietary support might also help reduce the risk of cervical cancer. A 2020 review published in Medicina found the intake of specific vitamins and various fruits and vegetables with multivitamins may suppress cervical cancer development.
"Vitamin C, vitamin A and folate-rich foods are beneficial in maintaining cervical health," Grover said.
Ensuring regular care is essential, Grover added. Be sure to get routine women's health checkups where the vaginal canal and cervix are examined for any abnormalities.
She said it is advised that girls and women receive the HPV vaccine, which protects against types 16 and 18, the ones responsible for the highest rate of HPV-related cancers. According to the CDC, HPV vaccines have the potential to prevent more than 90 percent of HPV-attributable cancers.
"Smoking and alcohol cessation has shown to be very instrumental, in addition to exercising more," Grover said.
A 2014 study examined smoking's impact on HPV and found it increased incidence and prevalence rates. For high-risk HPV infections, smoking increased persistence rates.
According to the WHO, effective intervention strategies could reduce the high global mortality rates from cervical cancer. Thanks to screenings and available vaccines, cervical cancer is one of the most preventable cancers.