The Prevalence and Risks of HPV

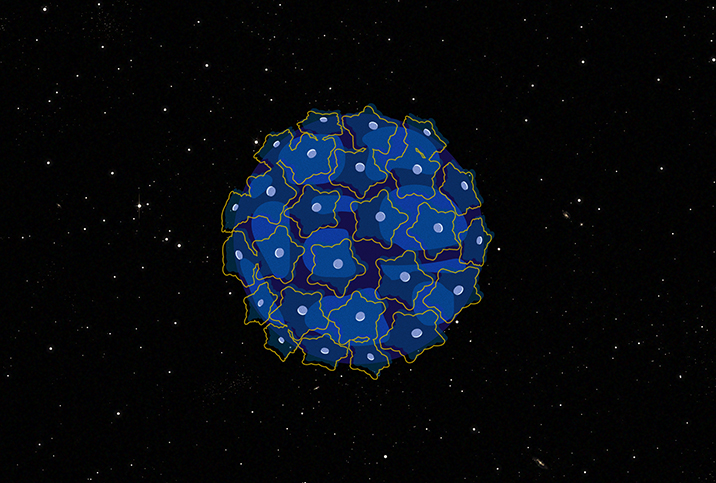
HPV is one of the most successful viruses in human history. There are more than 200 known subtypes and they are collectively referred to as the human papillomavirus.
"HPV is a double-stranded DNA virus. It only infects humans and there are more than 200 subtypes. Some subtypes cause skin warts of various kinds, while others infect anogenital region mucosal surfaces, such as the penis, scrotum, perineum, anal canal, perianal region, vaginal introitus, vulva and cervix," said Alex Polyakov, M.B.B.S., a senior clinical lecturer at the University of Melbourne and clinical director at the Royal Women's Hospital in Australia.
"Different subtypes of the virus cause different infection manifestations, ranging from benign warts to cervical and perianal cancer," he added. "So overall, clinical manifestations depend on the type of the HPV that is involved."
There are approximately 42.5 million active cases of HPV in the United States, which is about 1 in 8 people, according to the Centers for Disease Control and Prevention (CDC). In fact, the CDC claims HPV will infect nearly all sexually active men and women at some point in their lives.
Fortunately, the overwhelming majority of people who get infected are able to fight off the virus on their own within two years. Typically, this is done by the immune system before any visible symptoms present.
How it spreads and who's at risk
HPV has become so prevalent in society because it is highly contagious. And since most people are asymptomatic, the virus is passed on without any knowledge of their own diagnosis. This is especially true for people who are sexually active and have multiple partners.
"Everyone who has unprotected sex can catch HPV," according to Laurence Gerlis, M.A., M.B., the CEO and lead clinician at SameDayDoctor, a private general practitioner practice with clinics in London and Manchester in the United Kingdom. "The more partners you have and the more sex without a condom, the higher the risk of catching HPV."
Certain individuals are likely to be more at risk than others.
"HPV is the most common sexually transmitted infection," said Robyn Faye, M.D., a member of the Women's Health Advisory Council for the HealthyWomen website, based in Middletown, New Jersey. "The infection is higher in certain racial/ethnic groups and those who are immunocompromised, such as pregnant patients and those with HIV and undergoing cancer treatments or who have cancer."
Even though HPV is considered a sexually transmitted infection (STI), it doesn't actually require sex to be spread, as it can also be transferred through skin-to-skin contact with an infected person. No orgasm or genital penetration is required.
"HPV is a virus which is sexually transmitted or through other types of close contact," said Babak Ashrafi, M.B.B.S., B.Sc., from Superdrug Online Doctor, an online pharmacy based in the U.K. "Viral particles pass from one person to another through direct contact such as through anal, oral and vaginal sex. HPV is also spread very easily through prolonged intimate skin-to-skin contact, which means it can be transmitted during nonpenetrative sex such as hand-to-genital contact."
The majority of HPV transmissions usually occur during or shortly after sexually related activity. Condoms help reduce the risk of transmission, but experts say they cannot guarantee protection against HPV.
Facts, stats and studies
All the different variants of HPV share one trait: They infect what is known as the epithelium.
Epithelial tissue lines various cavities in our bodies, including the genitals, anus, throat and mouth. Human skin is made up of epithelial cells, and HPV can invade if allowed to enter through a wound or abrasion. Epithelial cells cover almost all external and internal surfaces in the body.
Although most people who have HPV are asymptomatic, a common symptom of HPV is warts. Although rare, an HPV wart outbreak could appear on your hands, feet, face, mouth, throat, genitals or anus. An outbreak certainly can be a nuisance, but it is an indication that you have a harmless variant of HPV. This is good news since some rare types of HPV can lead to cancer if given enough time.
HPV is responsible for about 50 percent of high-grade cervical precancers, according to the World Health Organization (WHO). The specific variants of HPV found in these cases are HPV types 16 and 18; genital warts are most commonly caused by HPV types 6 and 11.
High-risk variants of HPV (such as types 16 and 18) do not produce symptoms but may lead to cervical cancer in women. In fact, the CDC notes the virus is responsible for almost all cases of cervical cancer in the U.S., because HPV changes the structure of the epithelial cells that line the cervix walls, creating an abnormal transformation known as cervical dysplasia, which is a precancerous condition.
There are approximately 42.5 million active cases of HPV in the United States, which is about 1 in 8 people.
Cervical dysplasia is not cancer, but if left untreated, can lead to cancer. Removing or destroying these abnormal cells is a very effective treatment or countermeasure. Most people who develop cervical dysplasia do not develop cervical cancer, and if they do, it develops very slowly.
In order to detect HPV-related precancerous lesions early, experts recommend all women get regular Pap smears starting at the age of 21, repeating the procedure every three years until age 29.
A Pap smear doesn't stop cervical dysplasia, but it does identify its presence, allowing your healthcare provider to treat the condition before it can develop into cervical cancer. Protecting yourself from HPV by getting vaccinated is also an effective countermeasure; it is best to do this before infection.
HPV poses the highest risk to women due to the possibility of developing cervical cancer. Cancers of the vagina, vulva and oropharynx (back of the throat) have also been linked to HPV, but are much rarer in comparison.
Men may also develop cancers of the penis, anus and, most commonly, the oropharynx. However, all of these cancers are rare. A 2021 study published in the Journal of Lower Genital Tract Disease suggested gay men have a higher risk of developing HPV-related anal cancer when compared with the general population.
For men who have sex with men, your healthcare provider might suggest an anal Pap test. Similar to a cervical Pap smear, it can identify potential precancerous cell formations early on.
A weak immune system is vulnerable to infections
Remember that most people can naturally fight off an HPV infection without showing symptoms.
"While infection with different types of HPV is almost universal, most infections clear without any clinical manifestations," Polyakov explained.
However, people with weak immune systems may struggle.
"HPV is a virus, and like all viral infections, our immune system plays a huge role in fighting it. So if you have any condition which reduces your immunity or immune response, you might be at higher risk of more serious symptoms," Ashrafi said. "These conditions might include things like uncontrolled diabetes, hereditary conditions or being on cancer treatments."
It's important to get tested, as most HPV carriers are asymptomatic with no idea the virus is already in their system.
"Unfortunately, most people who have a high-risk type of HPV will never show any signs of the infection until it has already caused health problems," Faye noted. "You can develop warts or an abnormal Pap or abnormal cells years after having sex with someone who has had the infection. This makes it hard to know where you first got it. This is why regular checkups are so important: Testing is the only way to know for sure that someone is at risk."