The Insidious Interstitial Lung Disease
Interstitial lung disease (ILD) is an umbrella term for a large collection of connected lung problems that affect the interstitium, the tissue surrounding air sacs, blood vessels and airways in the lungs.
More than 200 lung disorders fall under interstitial lung disease, the most common of which cause progressive scarring of lung tissue. However, despite the wide variety of types, ILD is very rare, affecting between 2 to 20 per 100,000 people. Common symptoms of ILD include shortness of breath—at rest or during exertion—and a dry cough.
"This is a very diverse group of disorders that can range from inflammation to scarring [of the lungs]," said Stacey-Ann Brown, M.D., a pulmonologist and assistant professor of medicine at Johns Hopkins University in Baltimore, Maryland.
The most widely studied and common ILD is idiopathic pulmonary fibrosis (IPF), the word "idiopathic" meaning there is no known cause. IPF is more likely to progress than not, and for patients who have progressive IPF, the median survival rate is 2 to 5 years. However, some forms of ILD can stabilize.
"In extremely severe cases, patients may get very short of breath and may require oxygen around the clock," Brown said. "That's toward end-stage interstitial lung disease."
Despite the wide variety of types, ILD is very rare, affecting between 2 to 20 per 100,000 people.
Amy Hajari Case, M.D., a pulmonologist and senior medical advisor for education and awareness at the Pulmonary Fibrosis Foundation, noted that while most ILDs are idiopathic, a cause can be identified in about one-third of cases.
"The prognosis is incredibly variable, depending on the type of interstitial lung disease," Case added.
In addition to the typically idiopathic nature, Mark Yoder, M.D., a pulmonologist and associate professor of medicine at Rush Medical College in Chicago, Illinois, said ILDs tend to sneak up on patients.
"They don't just appear," Yoder explained. "They're very insidious."
What causes interstitial lung disease?
"The primary known causes of ILDs include rheumatologic conditions, and environmental and occupational exposures to drugs or inhaled toxins or pollutants," Yoder said. "Some of the known autoimmune diseases that can lead to interstitial lung disease include rheumatoid arthritis, scleroderma and myositis.
"With those diseases, we think the immune system that's causing arthritis or that's causing the muscle weakness or muscle pain, that inflammation is also happening in the lungs," Yoder added.
When examining a patient with ILD, Yoder noted that he makes sure to find out if they have any underlying autoimmune diseases.
Occupational exposures are known to cause ILD, too, and can include jobs like sandblasting or stone cutting. Demolition work that involves tearing down older buildings with asbestos can also potentially lead to ILD.
"A category of ILD known as hypersensitivity pneumonitis can be caused by exposure to allergens like mold or down pillows," Yoder said. "People who are very sensitive to these could develop the disease.
"I think with those individuals, it's clearly [that] the person genetically is wired to have a bad reaction to certain things," he clarified.
In a recent study in CHEST, the journal of the American College of Chest Physicians, researchers indicated that viral infections could lead to the development of interstitial lung disease, specifically idiopathic pulmonary fibrosis. So while the primary reasons for this collection of lung disorders remain unknown, scientists are at least discovering possible leads.
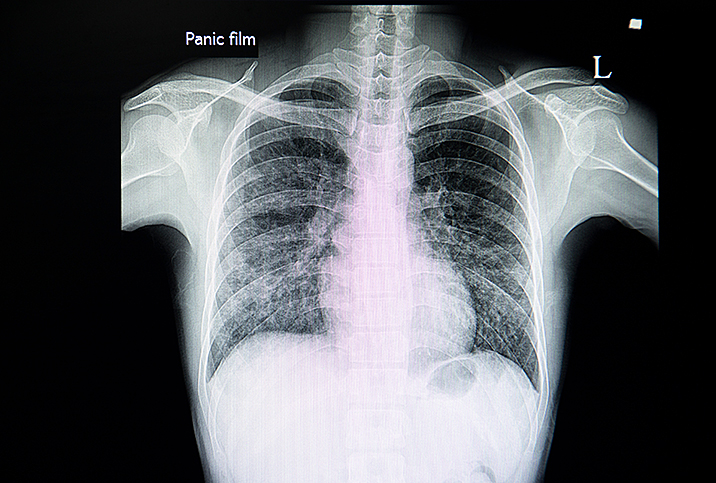
How is it diagnosed?
Brown noted that the most important diagnostic tool is history taking and a physical exam.
"We have to understand the chronicity of symptoms and if there is a cause or not," she explained. "You get that from the patient's story."
When listening to the lungs with a stethoscope, a doctor may hear crackles or rales—such as clicking, bubbling or rattling—in a patient with ILD.
"It sounds like crackling, like static," Brown said. Case agreed, noting that it sounds like you put your ear over a bowl of Rice Krispies with milk.
Once the pulmonologist has a reason to suspect interstitial lung disease, they will generally order a high-resolution CT scan of the lungs, which helps diagnose and detect patterns of lung changes that could be helpful in categorizing the type of disease.
The most important diagnostic tool is history taking and a physical exam.
If the imaging looks suspicious for a possible rheumatologic-associated ILD, the doctor may proceed to other diagnostic procedures. For some interstitial lung diseases, a bronchoscopy—involving placing a camera into the lungs—may be appropriate. Small biopsy samples, either of the lymph nodes or the lung itself, could also be necessary for another narrow subset of ILD, Brown noted.
"Another key diagnostic tool is a multidisciplinary review," Brown said, "which can include other medical professionals, like a thoracic radiologist, pathologist and rheumatologist. When a multidisciplinary group reviews the case, it can strengthen the diagnosis.
"It can be very difficult to make a diagnosis, even with a surgical biopsy," she added.
Case said the challenging part of making an ILD diagnosis is that the symptoms can be very nonspecific.
"It can actually be pretty subtle early on," Case said. "Most of the time people who have symptoms have a dry cough, shortness of breath—initially with exertion, but it can become progressive. They can have fatigue, they can have other more systemic symptoms, like loss of appetite, weight loss, weakness and discomfort in the chest. As you can imagine, those symptoms can show up in lots of different medical conditions."
What are the treatment options?
Treatment depends on the diagnosis and type of interstitial lung disease. With idiopathic pulmonary fibrosis, medications that reduce inflammation or suppress the immune system are not helpful and may prove harmful, Brown said.
There are two FDA-approved drugs for IPF: nintedanib and pirfenidone. These are antifibrotic agents, medications that slow the rate of the progression of scarring.
"For patients who continue to suffer a decline in lung function, even with the antifibrotics, a lung transplant may be considered. A lung transplant is the only curative treatment for advanced pulmonary fibrosis," Yoder said.
"Only a very small group of patients are sick enough to need a lung transplant but well enough to tolerate the surgery and ongoing immunosuppression," Brown clarified.
"They must have severely impaired lung function, but must have relative preservation in other organs, so no end-stage lung disease," she added. "At most lung transplant centers, the patient must be under age 70 and cancer-free."
Case stressed that a healthy amount of exercise, particularly a pulmonary rehabilitation program, can be beneficial for ILD patients.
"This is a structured exercise program that's monitored by physical therapists or respiratory therapists that can be individualized to a person's needs and help them progress in a way that's safe for them," she explained. "[This] can really help with their functional capacity and their symptoms and energy level."
Pay attention to symptoms
Yoder pointed out that the 2- to 5-year survival rate for idiopathic pulmonary fibrosis is probably not completely accurate—the prognosis is likely better.
"I think we're detecting these diseases earlier now, and we've gotten some treatments that can either stop them in their tracks or slow them down a lot," he said. "It's probably going to be much longer than that in the patients who we detect sooner and then also the patients who get on appropriate treatment."
However, Yoder confirmed that, with IPF, once scarring occurs, it's irreversible.
"Many patients, particularly those with an insidious onset of shortness of breath, may not pay attention to their symptoms early on," Case said. "Plus, people at a higher risk, such as those who smoke or work in professions that bring them in close proximity to hazardous materials, should talk to their doctors about potential risks regarding ILD.
"They'll rationalize it this way or that, or, 'Maybe I'm out of shape or getting older,'" she added. "It's really important to have our community—especially our primary care physicians—be thinking about interstitial lung disease, because if they don't, that diagnosis can easily be missed."