Gender Disparity Is Present in Cardiology Treatments
Gender bias in the healthcare community can be dangerous. New insights are revealing the disparity present in diagnosing and treating women, combined with a lack of understanding about the differences in symptoms and reactions to medications.
"More women than men die each year from a condition that is preventable 80 percent of the time," said Nitza I. Alvarez-Torres, M.D., a cardiovascular disease specialist and the president of the Tri-County Heart Institute, based in The Villages, Florida.
"We are underrecognized, underdiagnosed and undertreated as a consequence of this gap," Alvarez-Torres added.
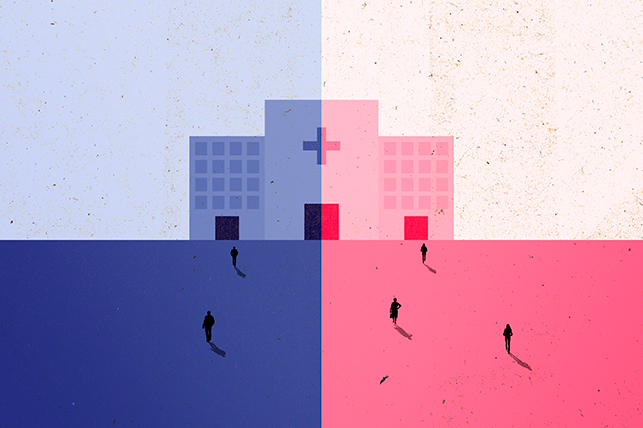
Bias in cardiology
Women are more likely to receive advice to lose weight, change their diet and start exercising to improve their cardiovascular health, while men are more likely to receive medication, according to a study presented in December 2022 at a congress organized by the European Society of Cardiology, the Asean Federation of Cardiology and the Asian Pacific Society of Cardiology.
The study results suggest differences in preventive treatments based on the misperception that men are at higher risk for heart disease. However, according to the American Heart Association, 1 in 3 deaths of American women are caused by heart disease—more than the rate for breast cancer.
Despite similar guidelines for men and women in heart condition prevention, men are typically prescribed lipid-lowering drugs, while women receive advice on lifestyle changes, study author Prima Wulandari, M.D., of Harvard Medical School and Massachusetts General Hospital in Boston, said in a statement.
Gap for proper prevention
"A change in lifestyle is important for everybody irrespective of gender. Unfortunately, due to the misconception that women have a lower risk for cardiovascular diseases, they don't receive proper evaluation or screening," Alvarez-Torres said.
According to Wulandari's study, compared with men, women were 38 percent more likely to receive exercise advice and 27 percent more likely to obtain weight-loss recommendations. In contrast, men were 20 percent more likely to be prescribed statins.
Prevention is the best intervention, Alvarez-Torres said.
"If we see the massive gap that this study reveals, that a preventive measure as simple as a cholesterol medication is not administered as indicated, how can we be successful in preventing heart attacks?" Alvarez-Torres asked.
Lack of proper evaluation, treatment and awareness are the reasons 420,000 women continue to die each year from heart disease, Alvarez-Torres said.
Representation in medical research
Historically, women have been underrepresented in research studies. Although this has been changing, it is still not enough. Much of the information currently available on symptoms, forms of diagnosis and response to medications is based on studies of men.
"In science, what we don't study, we don't understand," Alvarez-Torres said. "If we don't understand, we tend to ignore or just do whatever we think is best. And this is scary for us as women. As one of my friends will say, 'Were you born a woman? Better luck in your next life.'
"The lack of representation of women in cardiac research has perpetuated the lack of knowledge on accurate diagnostic tools, efficacy and safety of interventions in the female population," Alvarez-Torres explained.
Appropriate education
Significant differences exist between men and women, but less information about women's health has led to gaps in medical knowledge. Meanwhile, a lack of understanding of how diseases manifest contributes to delayed diagnoses for women.
When women exhibit symptoms of heart disease, they tend to be underdiagnosed and undermedicated compared with men, Alvarez-Torres wrote in her book, "Heels vs. Ties: Living With Your #1 Threat."
In this book, aimed at both a medical and nonmedical audience, she gathered current information and data on women's heart health, trying to clarify the differences and prevent more women from becoming statistics.
"Healthcare providers need to be educated on the differences...women are dismissed and trivialized because they are not necessarily presenting with chest pain," Alvarez-Torres told Giddy. "In our new chest pain guidelines, the word 'atypical symptoms' was removed, as there is clearly nothing atypical about the symptoms that a woman experiences."
Responses to drugs
Eight of 10 drugs withdrawn from the U.S. market between 1997 and 2000 posed major health risks to women, according to the U.S. Government Accountability Office. For its part, the U.S. Food and Drug Administration found women suffered more than 2 million adverse drug-related events between 2004 and 2013, compared with 1.3 million for men.
Women's Health Study, published in 2005, found low-dose aspirin used as a preventive therapy in women does not reduce the risk of first heart attacks. For years, this treatment had been considered because of the benefits in men. It is now known that more research is needed to understand the causes of the responses in women.
"As this disease was once thought to be a man's disease, almost everything that we know is extrapolated from man to woman, assuming that it was the same," Alvarez-Torres noted.
Inaccurate tests in women
Common methods for assessing cardiovascular disease risk have not been as effective in women, Alvarez-Torres explained. For example, women with heart attacks generally have less plaque in their arteries. This means a good result on a diagnostic test does not necessarily equal a healthy heart.
"The tests commercially available today were designed to detect plaque buildup in the arteries, the main cause of heart disease in men," Alvarez-Torres said, adding that although women can have this form of heart disease, others are undetected by these tests.
"The lack of awareness in this regard can make the physician falsely believe that a woman has no heart condition," Alvarez-Torres said. "As a consequence, she will not receive the proper treatment, and that can cost her life."
Stereotypical perceptions
According to several studies, the disparity in treatment is related to stereotypical views of pain: Women are seen as emotional by some healthcare providers, while men are labeled "courageous"; meanwhile, women receive less aggressive treatment until they can demonstrate the severity of their illness.
For heart disease, however, women may not present with pain and, for this reason, may be underestimated and underdiagnosed by physicians.
"If they wait for just chest pain, they will be missing a lot of women with heart conditions, and that can [cost] them their lives," Alvarez-Torres said.
When they do show signs of a heart attack, women are less likely to receive timely medication or therapy compared with men, Alvarez-Torres said.
Some physicians are uninformed about the differences in heart conditions between men and women. If you feel ignored by your healthcare provider, it's time to seek a second or third opinion.