Endometrial Stripe: Why is it Important and What You Need to Know?
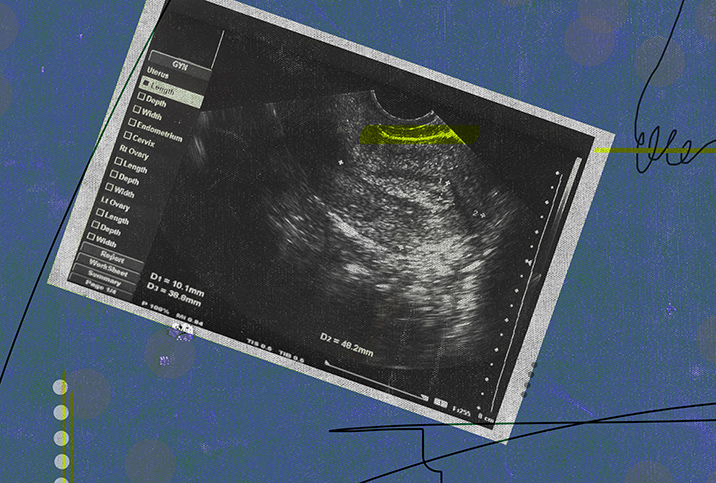
Ever wonder what the dark line is that appears on the screen when you have an ultrasound? Well, that line is actually known as the "endometrial stripe," and no, it doesn't have anything to do with endometriosis (although people often get them mixed up).
What is it? The lining of your uterus is called the endometrium or endometrial lining. This is a complex structure that allows for the implantation of embryos and aids pregnancy. Although tissue similar to the endometrium can grow outside the uterus, which is when conditions like endometriosis occur, the endometrial stripe refers only to that particular thick line you see on a scan.
What is considered normal endometrial thickness?
The thickness of this stripe can tell you a lot about your current stage of life. Tara Scott, M.D., an OB-GYN and the chief medical officer at Revitalize Medical Group in Akron, Ohio, explained what is considered normal endometrial thickness.
'Luckily, we have been able to identify this problem early on for most patients, and the majority of patients who get treated appropriately have an excellent prognosis.'
"For women still having menstrual cycles, the thickness varies depending on the time of your cycle. It can get as thick as 20 millimeters, and this is considered normal. We don't really remark on 'abnormal' levels if you are still cycling," Scott said. "For a postmenopausal patient who is having bleeding, the endometrial stripe should be 4 millimeters or less. But for a postmenopausal patient who is not bleeding, it can be normal to see an endometrial stripe of 7 millimeters, especially if they are taking HRT [hormone replacement therapy]."
According to an article published in the RadioGraphics journal, the average measurements of the endometrium can be 2 to 4 millimeters (mm) during your period, 5 to 7 mm during the early stage of your cycle (early proliferative phase) and up to 11 mm in the late stage (late proliferative phase). In the secretory phase, the thickness of the stripe can go up to 16 mm.
Does anything cause the thickness of your endometrium to change?
A number of factors can cause the thickness of your endometrium to change. Apurva Shah, M.D., a consultant OB-GYN at Tenet Healthcare in Boston, explained the causes of these lining thickness changes and when to be concerned.
"Any physiological or pathological conditions that impact the production of estrogen will affect the endometrial thickness. This includes aging leading to menopause, pregnancy, and conditions like PCOS [polycystic ovary syndrome] or obesity, both of which are hypoestrogenic states," Shah said. "Endometrial thickness is directly proportional to the amount of estrogen exposure to the uterus, which in turn is directly proportional to endometrial abnormalities, including cancer."
"Thickened endometrium is a sign of estrogen excess. When endometrial glands are exposed to excess estrogen, they proliferate beyond normal limits. This can lead to what is called hyperplasia, which is an abnormal proliferation of endometrial glands and often the first stop on the way to endometrial cancer," Shah continued. "Luckily, we have been able to identify this problem early on for most patients, and the majority of patients who get treated appropriately have an excellent prognosis. The most important takeaway point is to never ignore even the slightest bit of spotting in menopause."
Uterine cancer is one of the main types of cancer that affects women's reproductive organs, according to the Centers for Disease Control and Prevention (CDC). Uterine cancer is most commonly found in postmenopausal women and its symptoms include abnormal bleeding and discharge. If an ultrasound technician finds that your endometrial stripe is unusually thick (typically, more than 11 mm), they may refer you to a gynecologist for further testing to rule out endometrial cancer.
While a big, black stripe on a scan can often look daunting to patients, the endometrial stripe isn't often a cause for concern and is supposed to be there. But if you are showing unusual symptoms such as heavy bleeding, painful sex or bleeding after menopause, you should definitely consult your physician so they can rule out any serious issues.