Breast Calcifications Are Usually Benign, But Watch for Warning Signs

Breast calcifications are calcium deposits that develop in a woman's breast tissue. They usually show up as bright white flecks or spots on a mammogram, and are more prevalent in older women.
According to a 2013 study in the Journal of Clinical Imaging Science, only 1 percent to 2 percent of women under age 50 have breast calcifications, but by age 70, more than 50 percent of women will have developed this condition. Fortunately, breast calcifications are usually noncancerous.
"Calcifications tend to become more common with increasing age, but most of these will be benign," confirmed Richard Reitherman, M.D., Ph.D., medical director of breast imaging at MemorialCare Breast Center at Orange Coast Medical Center in Fountain Valley, California.
However, specific patterns of these calcifications may be indicative of invasive breast cancer, its noninvasive counterpart, ductal carcinoma in situ (DCIS) or a progression toward it. Read on to learn what experts say are the warning signs to look out for with this condition.
Causes and risk factors
The causes of breast calcification are not precisely known, but there are risk factors to be aware of, explained Kavita Jackson, M.D., an emergency physician and breast cancer survivor.
In addition to being more common with age, Jackson said, "Women who have previously had breast surgery, breast injuries, breast infections or breast cancer also seem to have a higher risk of developing calcifications."
"One could make a circular argument that women that have a higher lifetime risk of breast cancer (such as family history) would therefore have a higher risk of mammographic calcifications," Reitherman added.
Conditions that are commonly associated with breast calcifications and may be possible causes include:
- Invasive breast cancer
- DCIS
- Fibroadenoma, a type of noncancerous breast tumor
- Trauma from surgery or injury
- Infection
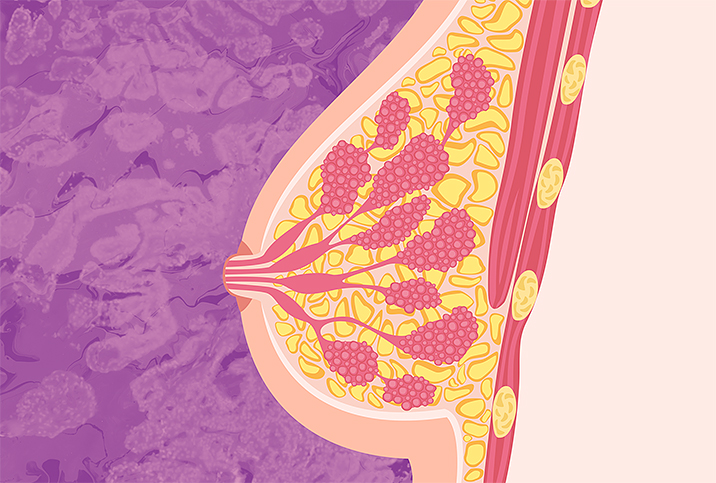
- Clogged milk ducts (duct ectasia)
- Breast cysts (fluid-filled sacs in the breast)
- Radiation therapy as a treatment for breast cancer
- Fat necrosis
It's important to note that mammographic calcifications are not related to calcium metabolism and are not in any way influenced by taking calcium supplements. Women who take supplements to treat osteopenia/osteoporosis are not at higher risk for breast calcifications.
Types of breast calcifications
There are two types of breast calcifications: macrocalcifications and microcalcifications. Of the two, microcalcifications are the more worrisome.
Macrocalcifications
These are coarser and larger deposits of calcium that cannot be felt from the outside. When seen on a mammogram, they look like white spots usually dispersed randomly within a woman's breast.
Macrocalcifications can be diagnosed without a biopsy and are usually associated with breast changes due to aging and the body's natural wear and tear.
Microcalcifications
Microcalcifications are more concerning because they can be malignant. They are extremely small in size, and when seen on a mammogram, appear as white specks.
If microcalcifications are identified, your doctor may require additional testing. When the calcium deposits look suspicious in size or appearance, a breast biopsy may be needed to rule out breast cancer. Certain patterns can indicate the breast calcifications may be early-stage breast cancer.
"The responsibility of the radiologist interpreting the calcifications is to determine whether they are benign (nonmalignant), are probably benign so that mammographic follow-up is recommended, or that the calcifications should be biopsied, using stereotactic technology," Reitherman explained. "Calcifications are analyzed based on the shapes, sizes and patterns displayed on the mammogram."
Breastcancer.org's website suggests calcifications are likely benign if they are larger than 0.55mm, do not cluster in a single area of the breast, and appear in standard shapes with well-defined edges. However, if they are smaller than 0.5mm, have varying sizes and shapes, and are clustered within a single area of the breast, they are considered suspicious and will require further testing.
Understanding the relationship between calcifications and cancer
While most calcifications are noncancerous, microcalcifications emerging in a certain pattern can indicate cancer.
"The calcifications themselves are harmless and the majority are benign," Jackson said. "Depending on the size or pattern of calcifications, they can raise concern for cancer. They are typically identified on mammograms, and a breast radiologist can determine whether further testing for cancer is warranted."
A 2017 study published in Scientific Reports highlights that we still have a poor understanding of breast calcification, but there is increasing evidence that calcifications are not "passive bystanders." In fact, they can be active participants in how breast cancer progresses.
"Most women will have calcifications appear on their mammograms at some point, and these will be benign and not requiring any further action," Reitherman said. "However, microcalcifications can be a result of a growing cancer. Either invasive or noninvasive (DCIS) can present as microcalcifications on a mammogram, although this is more commonly seen in DCIS."
However, in some instances, breast calcifications can be the exclusive sign of breast cancer.
A 2017 Breast Cancer Research and Treatment study indicated breast calcifications were the only sign of breast cancer in 12.7 percent to 41.2 percent of women who had post-mammogram testing. In addition, the researchers pointed out 54.5 percent of calcifications that turned into cancer could have been detected earlier, reiterating the importance of early diagnosis.
Next steps
It's important not to get ahead of yourself and immediately conclude cancer if your mammogram shows calcifications. Still, it's equally important to be proactive and monitor these breast changes, especially if you're considered to be high risk for cancer.
Although breast calcifications cannot be prevented, routine mammography is an important way to detect any potential cancer early.