Researchers Identify Possible 'Achilles Heel' of Ovarian Cancer
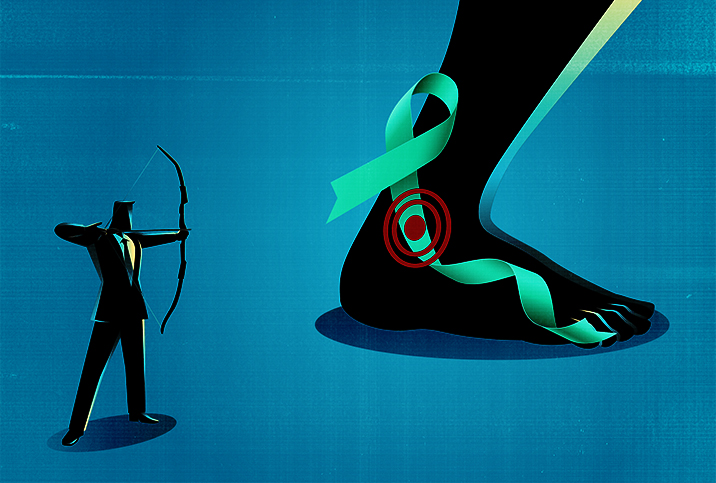
Scientists say a newly discovered cellular pathway that ovarian cancer cells use to survive, grow and spread could be targeted by cutting-edge treatments to help stop the disease in the future. By shining a light on the ways in which ovarian cancer cells evade destruction, researchers may have found the key to killing or stopping these cells in their tracks.
The research, led by W. Lee Kraus, Ph.D., of the University of Texas Southwestern Medical Center, was published in the August 2021 issue of the journal Cell.
"We've defined a new pathway that helps us understand the biology of ovarian cancer," said Kraus, professor and director of the Cecil H. and Ida Green Center for Reproductive Biology Sciences at UT Southwestern.
The work of Kraus' team, including lead author of the Cell study, Sridevi Challa, Ph.D., could eventually be the foundation for helping to choose and tailor therapy for ovarian cancer patients, so they achieve the best outcomes from their treatment.
Development of treatments that target the pathway and its associated biomarkers—therapies called PARP-16 inhibitors—is a hot topic in cancer research right now. They may hold promise for extending the lives of patients with even the toughest of cancers, including ovarian cancer.
Challa, a postdoctoral researcher at UT Southwestern, received a 2-year grant from the Ovarian Cancer Research Alliance to fund the work highlighted in the Cell study.
Born and raised in India, she came to the United States when she was 21 to work as a research technician. She then went on to attend graduate school, and now works exclusively in Kraus' lab at UT Southwestern with multiple research collaborators.
By shining a light on the ways in which ovarian cancer cells evade destruction, researchers may have found the key to killing or stopping these cells in their tracks.
"Receiving that fellowship meant a lot. I felt it was a validation of my work as an ovarian cancer researcher," Challa said in an interview for Giddy.
The Cell study describes the team's discovery of the ways in which ovarian cancer cells transform to survive when they are under stress from the accumulation of toxic proteins due to high levels of protein production.
"Many researchers are trying to find dependencies in cancers by asking why a cancer cell amplifies a gene, increases the level of a protein or upregulates a critical cellular pathway," Kraus explained. "These changes give that cancer cell a selective advantage to survive in conditions of stress, but at the same time, they can become an Achilles heel—something that, if the alteration was blocked, would kill the cancer or stop its growth."
Therapies like PARP-16 inhibitors might be able to effectively stop the biological changes the researchers discovered that make ovarian cancer cells so powerful. These inhibitors could be another weapon in the arsenal to treat ovarian cancers, perhaps providing a different approach for cancers no longer responsive to current drugs.
If validated, this research may one day help oncologists select which ovarian cancer patients will benefit most from PARP-16 inhibitors, which are now in development. No PARP-16 inhibitor drugs are yet in clinical trials or approved by the FDA.
In their research, Kraus and his colleagues determined ovarian cancers massively increase an enzyme called NMNAT-2. This enzyme makes NAD+, an enzyme important for the family of enzymes known as PARPs, which play an important role in the growth and metastasis of some cancers.
In the Cell study, the research team showed that in ovarian cancer, a PARP enzyme called PARP-16 uses NAD+ to modify ribosomes, crucial protein synthesizing machines of the cell.
The result is a decrease in the production of new proteins, which is important for cell function. The cell can then fine-tune itself to prevent toxic proteins from collecting and killing the cell.
The research team identified two biomarkers for ovarian cancer, including mono(ADP-ribose)—a modification mediated by some of the PARP enzymes including PARP-16—and the enzyme NMNAT-2.
"When we looked at pathological samples of ovarian cancer, there was a very strong correlation between the presence of mono(ADP-ribose) and worse patient outcomes," Kraus explained.
"Our finding could also be relevant in other cancers with high NMNAT-2 levels, such as neuroblastoma," he added.
Current PARP inhibitors, which are all aimed at the PARP-1 enzyme, have no power against the pathway and biomarkers discovered by Kraus and colleagues. But PARP-16 inhibitor drugs, now in early phase development, could be effective deterrents.
PARP-16 inhibitors could eventually be used in combination with already existing drugs as weapons against ovarian cancer, according to Kraus and Challa.
Challa noted the grant from the Ovarian Cancer Research Alliance that funded this study will also be used to delve into the question of whether their discovery could be used to help develop new cancer therapies.
Challa was motivated to pursue cancer research as a vocation and field of study because she saw firsthand how cancer affected members of her own family. When she was 4 years old, her father died of esophageal cancer at age 42.
"When I was younger, people would say that cancer occurs in people who have bad habits like smoking. But that's not always true. It didn't seem to me that people understand a lot about cancer," Challa said.
"Even if people are cured of cancer, there is a lot of financial burden from a diagnosis. Families are never the same afterward," she added.
Challa decided to research ovarian cancer, since it is so difficult to detect—and often a "silent disease" that primarily affects women.
"I felt there was a lot of need for early detection of ovarian cancers," she explained. "My hope is that someday my work will help at least one person with cancer. That drives my motivation to continue my research every day."