Intrauterine Insemination Gives Sperm a Much-Needed Head Start

For a couple trying to conceive, discovering a partner's sperm cells are not quite up to snuff can be a major disappointment. However, modern science has given couples several ways to overcome such obstacles.
Rudimentary artificial insemination dates back more than 200 years, and modern assisted reproductive technology (ART) has been around for decades, with in vitro fertilization (IVF) being the best known. A method with a longer history but less popularity than IVF is called intrauterine insemination (IUI), a procedure that can help get the most out of a guy's gametes, if they're the problem.
Sukhkamal Campbell, M.D., M.S.C., is the director of fertility preservation services in the obstetrics and gynecology department at UAB Medicine in Birmingham, Alabama. When a couple struggles to conceive and Campbell is trying to find out why, she considers three broad categories that often contain the answer: eggs, the uterine cavity and sperm. When the first two are OK, focus moves to the sperm, about 15 million to 200 million of which are typically contained in every milliliter of semen. These male reproductive cells remain crucial for conception. If they're underperforming, IUI is an option many couples pursue.
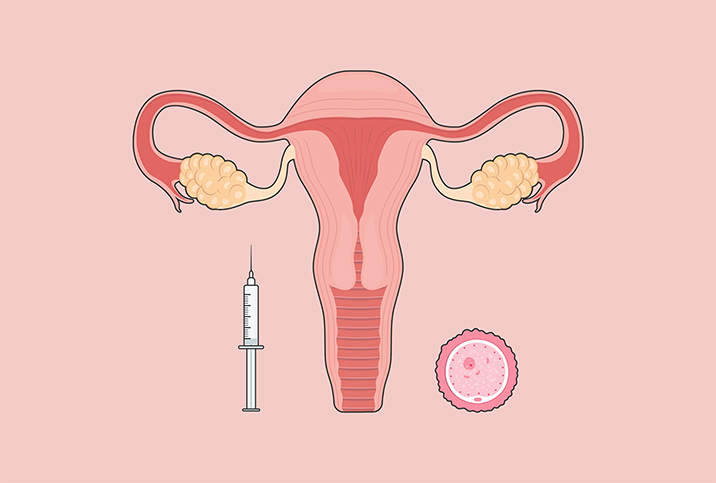
"Intrauterine insemination is a procedure where we take our prepared sperm specimen and, basically, place it directly into the uterine cavity to pass the cervix," said Emily Jungheim, M.D., M.S.C.I., the chief of reproductive endocrinology and infertility in the obstetrics and gynecology department at Northwestern University's Feinberg School of Medicine in Evanston, Illinois.
Campbell explained IUI in more detail: Washed, processed and concentrated sperm—from a male partner or a donor, which is common with IUI—are injected into the uterus of the recipient via a flexible catheter that goes through the cervix. This action effectively places the sperm near the egg to facilitate fertilization, with luck.
Historically, Jungheim said, she's seen couples in her practice turn to IUI after attempts to conceive through intercourse without medical help failed.
Male-factor issues and considerations
While 8 percent to 12 percent of couples worldwide experience fertility problems, up to half of all infertility cases are attributed to male-factor issues and, according to the authors of a 2015 review of literature, up to 2 percent of all men "exhibit suboptimal sperm parameters."
If intercourse fails to result in a desired pregnancy, a semen analysis can determine the presence, quantity and movement (motility) of sperm, Jungheim said. Campbell highlighted morphology, which refers to a measure of the sperm's ability to fertilize eggs and is based on how the sperm looks in comparison to the norm.
Fertility specialists and clinics use different thresholds when deciding how much sperm is sufficient to make IUI viable.
"If there are no motile sperm present, it doesn't make sense to do an IUI," Jungheim said. "If you look at a semen analysis and you see that there are at least 10 million motile sperm present in that analysis, it's reasonable to proceed with an insemination and try it."
Pregnancy rates are highest with a post-wash total motile sperm count (TMSC) of 9 million or more, below which the rates decline in a linear fashion, according to results of a 2021 study published in the journal Fertility and Sterility that involved almost 38,000 patients and more than 92,000 insemination cycles.
Campbell emphasized that men providing IUI samples can optimize fertile health by limiting or eliminating exposure to toxins and substances such as tobacco, marijuana, alcohol and illicit drugs. Exogenous steroids like testosterone supplements can interfere with the internal production of the hormone essential for making sperm, possibly resulting in a remarkably low count if they are not prescribed by a physician who monitors the effects on the body, she added.
Abstaining from sex and masturbation during the "optimal window," which is two to seven days prior to providing a sample for analysis or IUI, is advantageous for fertilization, according to Campbell.
Gathering and preparing the sperm
The partner providing the sample for IUI collects the sample through masturbation either at home or at an office, and some offices have a collection room, Campbell explained. At-home collections can involve intercourse, using a special device, not a condom, Jungheim said.
Ideally, patients should bring samples from home to the clinic within 30 to 45 minutes following collection, Campbell said. Once the sample is at the office, clinicians take about 30 to 60 minutes to prepare it.
"It may be that the male partner is just dropping that specimen off and then the female partner is coming in an hour later," she added. "So it can be different in that they're not together for that."
The collected sample is given to an andrology team for semen analysis, which measures sperm parameters including total sperm counts and motility, Campbell said.
Labs process sperm samples using a gradient technique—sometimes called "washing"—or by way of a swim-up modality, or with the standard wash method most commonly used for IUI.
"The reason you need to wash it is because there are prostaglandins in the semen, and if that's placed directly into the uterine cavity, it can cause really horrible cramping," Jungheim said, adding that unwashed semen frequently available from donor sperm banks can be used for intravaginal administration and intracervical insemination, but not for IUI.
Proceeding with the procedure
Fertility doctors and patients planning for IUI monitor for ovulation with either a home ovulation prediction kit or ultrasounds to track follicular development and to figure out when it makes sense to do the insemination.
"The procedure itself, what it entails is placing a speculum, and then a catheter is gently placed into the uterine cavity," Jungheim said. "[For] some women, it can be difficult to get that catheter into the uterine cavity, and what I typically tell my patients is these instruments aren't one size fits all. We all have different natural curves and turns to our bodies, and so sometimes we need to use an ultrasound to find the correct path to get that catheter in. But overall, it shouldn't hurt."
According to Campbell, once all the informed consent and documentation is done, a sperm recipient begins the process by lying down on an exam table with their feet placed in stirrups. The recipient is often asked to maintain a full bladder to help flatten the uterine contour and straighten the cervix angle for ease of access and insertion.
"The sample is loaded into the catheter and attached syringe, and then the cervical canal is navigated and traversed with the catheter," she said. "Once the catheter has passed into the uterine cavity, the sample is injected and the empty catheter and syringe are withdrawn from the cervix."
After that, Campbell indicated the IUI specialists remove the speculum and take the patient's feet out of the stirrups, placing them flat on the table. The patient is asked to lie there for five to 10 minutes before leaving the clinic.
Prolonged rest following insemination is not necessary.
"Once the sample is inside of the uterine cavity, it's in," Jungheim said. "The uterus is an amazing organ."
She said her patients often report feeling fluid dripping and worry that the sample is seeping out, but the sensation is likely from the water used to rinse off the speculum, and the uterus reliably holds the sperm in place. Patients can get up and do whatever else they have planned for the day.
Campbell encourages recipients with a male partner to have intercourse the same day, if possible, because it introduces seminal fluid that potentially contains fertilization-friendly nutrients.
Conception still hinges on ovulation
Even with a boost from modern medicine, pregnancy is still predicated on ovulation, and timing is critical. Yet IUI affords a little leeway.
"So let's say you get a surge on your ovulation prediction kit on a Saturday; it may still be reasonable to do an insemination on a Monday," Jungheim said. "A lot of folks get really, really nervous about the timing, and I get that. And there is some importance to the timing. But it's not like in vitro fertilization where it has to be spot on. There's a little bit more flexibility there."