Exploring the Differences Between IUI and IVF

Confronting the idea you'll need intervention to get pregnant can be emotional and overwhelming. Luckily, an abundance of treatment options is available these days to make the dream of expanding your family a reality.
Of those available treatments, the two most common procedures remain intrauterine insemination (IUI) and in vitro fertilization (IVF).
The IUI process
IUI is the lower intervention option of the two procedures. The IUI procedure is timed specifically around when you're ovulating. Depending on your fertility and your family-planning goals, your doctor may put you on medication to help you ovulate or produce more follicles (eggs), thus increasing your chance of getting pregnant.
Your doctor will do ultrasounds of your developing follicle(s) every day from cycle day 10 onward until the follicle(s) mature. At that point, you will inject yourself with a "trigger" shot, which will cause you to ovulate approximately 36 hours later.
IUI is a simple procedure that can even be performed in the doctor's office without sedation. First, your partner provides a semen sample that is washed to remove the seminal fluid and low-quality sperm. Alternatively, frozen donor sperm is thawed and prepared. The sample is then injected into the uterus using a thin catheter, depositing the sperm close to the egg, by the fallopian tubes, which is where fertilization takes place.
The IVF process
IVF is a much more intensive process, as it takes about three weeks from start to finish, said Gopika Nandini Are, M.D., an OB-GYN in Garden City, New York. First, your cycle begins by using synthetic hormones to stimulate your ovaries to produce more eggs.
Multiple eggs are desired in an IVF cycle because not every egg will fertilize or develop. The synthetic hormones you'll be prescribed will likely be injectable and you'll have to perform the injections on yourself for one to two weeks.
Your doctor will be monitoring the development of eggs in your ovaries, and when they're satisfied with the maturation of the follicles, they'll instruct you to take a "trigger" shot that will help the eggs mature. The next day you'll go to your doctor's office for the egg retrieval. You'll be sedated while your doctor uses a transvaginal ultrasound to identify your eggs. Then, the doctor will use a small needle connected to a suction device to collect the eggs.
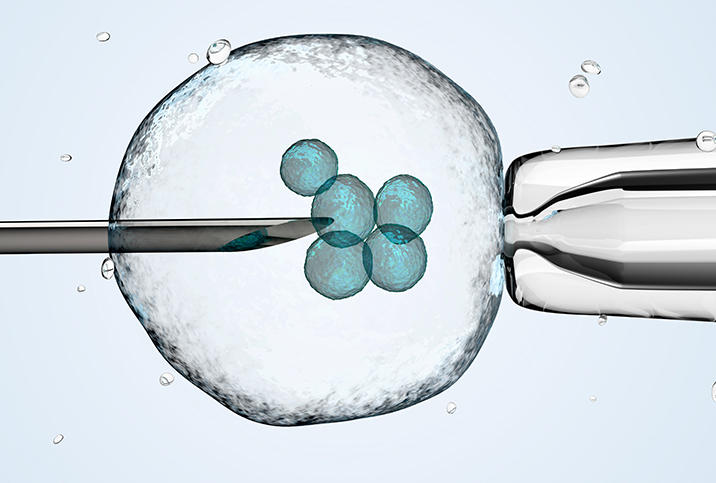
After all your eggs are retrieved, the healthy, mature eggs will be introduced to sperm—whether from your partner or a sperm donor—to hopefully create embryos. If you and your partner are struggling with low sperm count or motility, your doctor will likely suggest intracytoplasmic sperm injection (ICSI) at this stage, where a single healthy sperm is injected into each healthy, mature egg.
The eggs that have been successfully fertilized are now embryos, and they're left to incubate for two to five days. At that point, you will go to the clinic to have the embryos transferred back into your body via a catheter. The number of embryos you transfer depends on many factors, such as your pregnancy history, your overall health and your openness to a multiples pregnancy, Nandini Are said.
Which procedure is right for you?
Couples often start their infertility journey with IUI, because according to Nandini Are, IUI is "less invasive, significantly cheaper than IVF and a good fit for many types of infertility."
Good candidates for IUI include couples with unexplained infertility, ovulation disorders, suboptimal sperm counts and polycystic ovarian syndrome, and same-sex couples.
Depending on the severity of the infertility factor(s) and the health of the patients, success rates can be up to 25 percent per cycle. There's no requirement to start with IUI, unless it's required by an insurance carrier before it will cover IVF, according to Rebecca Pierson, M.D., a reproductive endocrinologist and fertility specialist with Indiana University Health in Indianapolis.
Good candidates for IVF include couples who have moderate to severe male-factor infertility, fallopian tube damage or blockage, endometriosis, previous tubal ligation or have otherwise not successfully gotten pregnant after three cycles of IUI.
"We also use IVF for couples when both partners have ovaries and they would like to have the egg come from the partner who is not carrying the pregnancies...or used when a couple or woman desires to use a gestational surrogate," Pierson said.
The live birth rate for the first cycle of IVF is 29.5 percent, though that number jumps up to a 54.5 percent chance of success when considering all embryos resulting from the first egg retrieval for women ages 35 and under, according to a 2015 JAMA study.
How the costs stack up
The costs of the two treatments vary widely—not just from each other, but depending on whether you're in an area with a high cost of living and whether your health insurance covers any of the treatment.
There are three main factors that determine the cost of an IUI: the medication used to stimulate egg development, the ultrasound monitoring and bloodwork, and the actual insemination. This procedure typically runs between $300 and $1,000, according to Planned Parenthood.
IVF has many more factors to consider when determining the final cost. There are the medications, ultrasound monitoring and bloodwork, egg retrieval, anesthesia, laboratory fees, cost of embryo storage and more to consider. All these costs add up to a range of $12,850 to $24,250, depending on the region, individual needs and your insurance coverage.
In the end, you have a lot of different options for fertility treatments, but IUI and IVF are two of the most common. Your doctor can help you determine which treatment is best for you and your family-planning goals.