Why Does My Clit Hurt?

The clitoris is the only organ in the human body that exists exclusively for pleasure. Unfortunately, it can also become a source of discomfort and pain for some women. Pain in the clitoris can happen for many reasons, here are nine of the most common.
What is the clitoris?
"The clitoris is part of the vulva, so anything which affects the health of the vulva can affect the clitoris," said Deborah Lee, M.B.Ch.B., a sexual and reproductive health specialist at Dr. Fox, an online pharmacy based in the United Kingdom.
"When thinking about diseases of the clitoris, it's important to remember the clitoris consists of smooth muscle, connective tissue, epithelial tissue, blood vessels and nervous tissue,” Lee said. “Disorders of any of these structures result in pathological changes and clitoral disorders."
This part of the body is also hormone-controlled.
"The clitoris is also under the control of hormones such as estrogen and testosterone, and raised or lowered levels of these hormones affect clitoral health, size and function," Lee added.
9 Types of clitoral conditions
Various disorders directly or indirectly affect the vulvovaginal area, including the clitoris. The following list is not comprehensive but covers some of the most prevalent health conditions that cause discomfort, irritation or pain in the clitoris.
Clitorodynia
Clitorodynia, or pain in the clitoris, is technically a symptom, not a disorder. But it is one of the most common reasons patients seek help from her practice, said Heather Jeffcoat, D.P.T., president of the Academy of Pelvic Health Physical Therapy and owner of Femina Physical Therapy in California. It is a subtype of vulvodynia (vulvar pain), she explained.
This symptom can arise from many causes, including localized conditions of the vulvovaginal area–such as an overabundance of nerves or disorders such as endometriosis, painful bladder syndrome, or hormonal insufficiencies, Jeffcoat continued. Sometimes, something as simple as a shower or if you wear tight clothes can cause pain.
Jeffcoat said that hypertonic pelvic floor muscle dysfunction, where the pelvic floor muscles spasm or are constantly tight, can cause issues too. This can result from direct trauma to the pelvic floor muscles or another injury, inflammatory process, orthopedic condition, or dysfunction–such as prolapse–that affects the pelvic floor.
Treatment depends on the cause. Medications and pelvic floor physiotherapy, or pelvic floor physical therapy, may be beneficial to help treat pelvic pain.
Clitoral atrophy
Clitoral atrophy indicates a clitoris that has shrunk in size, said Michael Krychman, M.D., an OB-GYN at HerMD in California. Orgasm intensity and the ability to become aroused are lost or diminished.
"Peri and postmenopausal women often suffer from vaginal dryness and soreness due to a precipitous drop in estrogen levels as they approach and pass through menopause," Lee said. "Due to low estrogen levels, the vulvovaginal epithelium becomes thin, flat and atrophic. It also becomes less sensitive, and all of this can affect sexual function."
Sometimes, the cause may be a side effect. Besides the natural effects of menopause, over 300 medications can cause vaginal dryness and contribute to clitoral atrophy, Krychman said.
Generally, Krychman and Lee said, topical estrogen creams and ointments can alleviate symptoms. Speak with your doctor to figure out a diagnosis and treatment plan if you experience dryness in your vaginal tissues.
Clitoromelagy
Clitoromegaly is an unusually large clitoris. Although the clitoris naturally swells during arousal, it resumes its usual size when the arousal state is over. In people with clitoromegaly, the clitoris remains enlarged for reasons unrelated to sexual arousal or stimulation.
According to Cleveland Clinic, the condition can be congenital or occur later in life. It typically occurs when a person assigned female at birth is exposed to excessive androgens, or sex hormones such as testosterone, that are more abundant in people assigned male at birth.
Sometimes it might be a symptom of congenital adrenal hyperplasia, or a macroclitoris, where the clitoris resembles a small penis. Clitoral priapism is an uncommon cause of clitoromegaly where the clitoris becomes engorged and painful and remains so for days or more.
It's thought to result from changes in blood flow, according to a report published in the Western Journal of Emergency Medicine and may occur as a side effect of certain medications.
Cortisone creams may alleviate clitoromegaly caused by inflammation, while hormone therapy can help with hormonal imbalances and adrenal dysfunctions, according to Cleveland Clinic. If priapism is a side effect of a medication, a doctor might suggest changing medications.
Vulvar dermatitis
An allergic reaction, or vulvar dermatitis, which affects the skin of the vulvovaginal area, isn’t uncommon. Seventy percent of women experience itching. Other symptoms include irritation and soreness.
"The vulvovaginal (VV) skin is thin, delicate and sensitive. The vagina has a very sensitive ecosystem," Lee said. "Female hygiene products often contain ingredients which cause contact (allergic) dermatitis to the VV skin, including the clitoris."
To avoid allergic reactions, most gynecologists advocate using cool water alone to wash the outer vulvovaginal area, including the labia and clitoris, Lee and Krychman said. Skip the soap unless it’s fragrance-free and hypoallergenic. Lee said soaps and other cleansers aren't necessary and can even be harmful.
Krychman and Lee explained that perfumes and other additives can spur an allergic reaction and disrupt the vaginal pH, increasing the risk of adverse skin conditions such as irritation and yeast infections.
Treatment can include prescription anti-itch medications, emollients and corticosteroid ointments. Contact your doctor to learn the right treatment method for your needs.
Vaginal infections
Infections affecting the vulva and vagina frequently impact the clitoris, Lee and Krychman said. The most prevalent of these are candidiasis (yeast infections) and bacterial vaginosis. If you are sexually active, you’ll need to pass on sex until after you’ve treated your yeast infection. It can be passed to your partner.
These uncomfortable infections aren't classified as STIs. Chlamydia, gonorrhea, herpes, syphilis and urinary tract infections can affect the clitoris as well, Lee said.
Common symptoms include:
- Pain
- Burning
- Itching
- Discharge
- Redness
- Discomfort during intercourse
The list of things to avoid is long: soaps, inserting a tampon, or using other perfumed feminine hygiene products. Skip over any products using colors, flavoring or other artificial additives.
To help reduce the risk of infections, consider the following advice:
- Don't douche: Lee explained douching could disrupt the vaginal microbiome, the colony of mostly beneficial bacteria that naturally inhabit the vagina, making it susceptible to candida overgrowth and other issues.
- Stay dry: Bacteria and fungi thrive in moist environments, so immediately change out of sweaty gym clothes and wet swimwear. Wearing loose-fitting clothing and cotton underwear can help.
- Use a water-based, glycerin-free lubricant: Like glucose (sugar), glycerin and other components in some lubes can increase the likelihood of both yeast infections and bacterial vaginosis, according to research.
- Watch what you eat: Excess sugar can increase the risk of a yeast infection, while eating probiotic foods and staying hydrated can support a healthy microbiome.
If you suspect you have a yeast infection or bacterial vaginosis, see a doctor for a correct diagnosis. Generally, over-the-counter antifungal creams or oral prescription medications can clear up the former, while antibiotics are needed for bacterial vaginosis.
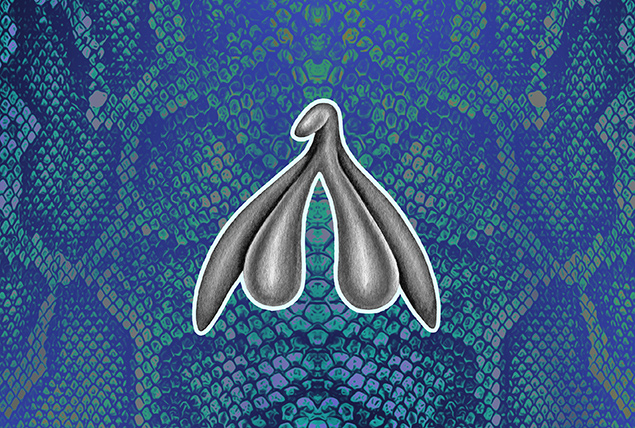
Clitoral adhesions
Clitoral adhesions are when the preputial skin adheres to the glans clitoris, Krychman said. One common iteration is clitoral phimosis, an anatomical condition in which the hood of the clitoris is too tight or there is no opening for the clitoris glans to protrude.
Some people are born with clitoral phimosis, while others acquire it through trauma (usually in childbirth), vulvar atrophy caused by estrogen deficiency, lichen sclerosis or chronic inflammatory dermatitis.
Depending on the severity, clitoral adhesions can cause discomfort, difficulty with arousal, pain and muted or absent orgasms, Jeffcoat and Krychman said. There are treatment options.
"To treat clitoral phimosis, external connective tissue and gentle adhesion releasing techniques are utilized to improve clitoral hood mobility," Jeffcoat said.
Surgery may be necessary in severe cases.
Autoimmunity
Lichen sclerosus and lichen planus are inflammatory dermatological conditions of the vulva. Lichen sclerosus can cause a host of symptoms, including severe inflammation, scarring, fibrosis or adhesions in the vulvovaginal area.
"The clitoris can become completely buried, and there can be local retention cysts," Lee said.
Lichen sclerosus can also cause thick, patchy, discolored skin around the genitals.
Lichen planus causes lacy white patches and painful sores in the vulvovaginal area, Lee said. Sores can last for months and make sex incredibly painful. Ulcers may appear in the mouth. On the skin, lichen planus can appear as purplish, flat and itchy bumps.
There is no cure for either disease, though steroid medications can remediate symptoms of both, Lee said. Surgery may be necessary in severe cases of lichen sclerosus to resolve adhesions
Nerve damage
Pudendal neuralgia or damage to the pudendal nerve, a major pelvic nerve, most often occurs due to childbirth or gynecological surgery. Strenuous physical activities such as hard bike riding or weightlifting can cause damage. This condition may arise from lumbar disc prolapse or spinal stenosis. Physicians don’t always know the cause.
In addition to pain and burning in the vulvovaginal area, injury or irritation to this nerve can cause urinary and fecal incontinence, Lee said.
"Nerve damage is difficult to treat as once the nerve is damaged, it is usually not repairable," she continued. "Pelvic floor physiotherapy may be helpful. Surgery, for example, spinal cord decompression in spinal stenosis, may be needed." Pudendal nerve blocks may help relieve pain.
Vulvar intraepithelial neoplasia (VIN)
Abnormal tissue development, or vulvar intraepithelial neoplasia, appears on external genitalia, such as the clitoris and surrounding area. Typically, it's caused by human papillomavirus (HPV) and may appear alongside genital warts. Some people with VIN experience no symptoms, while others experience itching, soreness and painful sex, Lee said.
According to the Royal United Hospital Bath, VIN isn't necessarily a precursor to cancer, though most gynecologists agree there is some associated risk. A doctor will likely perform an internal exam, take a biopsy to test for precancerous or cancerous cells and recommend routine cervical swab tests.
If VIN causes uncomfortable symptoms, a healthcare provider might recommend a topical steroid treatment to relieve inflammation and itching. A doctor can surgically remove the affected tissue in severe instances or where precancerous or cancerous cells are present, per the American College of Gynecologists and Obstetricians (ACOG).
Getting the HPV vaccine, practicing safe sex and avoiding cigarette smoking can all decrease the risk of HPV and subsequent complications, including VIN and vulvar cancer, according to ACOG. Share any unusual changes with your doctor, such as bleeding, ulcers and lumps.
The bottom line
When you experience pain in your clitoris, you don’t have to grit your teeth and bear it. Speak with a healthcare professional for the correct diagnosis. Some treatment options may be as simple as visiting a physical therapist or changing the type of feminine hygiene products you use.